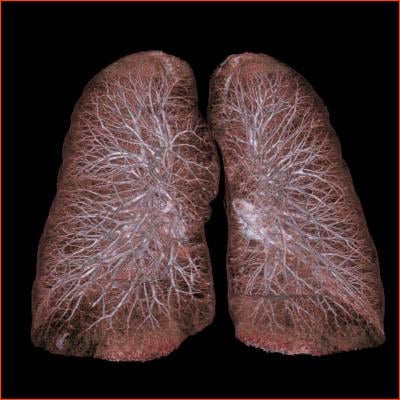
January 27, 2016 — Expanding lung cancer screening to include people who quit smoking more than 15 years ago could detect more cases and further reduce associated mortality, according to a study by Mayo Clinic researchers published in the Journal of Thoracic Oncology.
“A decline in smoking rates has been, and continues to be, a critical step to reduce lung cancer risk and deaths,” said the study’s lead author Ping Yang, M.D., Ph.D., an epidemiologist at Mayo Clinic Cancer Center. “But, it also means that fewer people have benefited from early detection of lung cancer, because more patients don’t qualify for low-dose CT [computed tomography] scans.” The current lung cancer screening criteria set by the U.S. Preventive Services Task Force (USPSTF) recommends CT screening for adults between the ages of 55 and 80 who have smoked at least one pack a day for 30 years and are still smoking, or have quit within 15 years.
In a study published in JAMA in 2015, Yang and her colleagues found that two-thirds of patients in the United Stats with newly diagnosed lung cancer would not meet the current USPSTF screening criteria, suggesting a need to adjust the definition of patients at high risk.
In the current study, Yang and her colleagues set out to identify which specific populations of individuals are at risk, but are being missed by the current lung cancer screening criteria. Researchers retrospectively tracked two groups of people with lung cancer: a hospital cohort made up of 5,988 individuals referred to Mayo Clinic and a community cohort consisting of 850 residents of Olmsted County, Minn.
They found that, compared to other risk categories, patients who quit smoking for 15 to 30 years accounted for the greatest percentage of patients with lung cancer who didn’t qualify for screening. The newly defined high-risk group constituted 12 percent of the hospital cohort and 17 percent of the community cohort.
“We were surprised to find that the incidence of lung cancer was proportionally higher in this subgroup, compared to other subgroups of former cigarette smokers,” said Yang. “The common assumption is that after a person has quit for so many years, the lung cancer rate would be so low that it wouldn’t be noticeable. We found that assumption to be wrong. This suggests we need to pay attention to people who quit smoking more than 15 years ago, because they are still at high risk for developing lung cancer.”
Equally important, the current study found that expanding the criteria for CT screening would not significantly add to the number of false-positive cases and would save more lives with an acceptable amount of radiation exposure and cost. Yang and her colleagues showed that expanding the criteria to include this risk category could add 19 percent more CT examinations for detecting 16 percent more cases. They calculated the expansion would result in minimal increases in false-positive results (0.6 percent), over diagnosis (0.1 percent) and radiation-related lung cancer deaths (4 percent).
"Lung cancer rates are dropping, because smoking is decreasing, but that doesn’t mean that our current screening parameters are good enough,” Yang said. “It is understandable, because the relative importance of risk factors changes over time. We need to adjust screening criteria periodically, so we can catch more lung cancers in a timely fashion. Based on our data, which are more recent and come from a well-defined population, I think that we should take action to screen this group, which is at high risk of developing the disease.”
She recommends additional research to confirm if similar trends are being seen in populations beyond Olmsted County, Minn. If confirmed, she recommends that policymakers consider changing the lung cancer screening guidelines to include people who quit smoking more than 15 years ago. She also recommends that policymakers continue to re-examine lung cancer screening criteria to account for changes in groups that are most at risk.
Co-authors are:
- Jason Wampfler, Mayo Clinic;
- Shawn Stoddard, Mayo Clinic;
- David Midthun, M.D., Mayo Clinic;
- Yi Wang, M.D., Wenzhou Medical University, China;
- Dong Xie, M.D., Ph.D., Shanghai Pulmonary Hospital, China; and
- Jun She, M.D., Ph.D., Shanghai Respiratory Institute, Fudan University, China.
For more information: www.mayoclinic.org


 April 17, 2024
April 17, 2024