October 25, 2016 — For men with intermediate-risk prostate cancer, radiation treatment with brachytherapy alone can result in similar cancer control with fewer long-term side effects. The findings come from research presented at the 58th annual meeting of the American Society for Radiation Oncology (ASTRO) comparing brachytherapy alone to more aggressive treatment that combines brachytherapy with external beam therapy (EBT).
NRG Oncology/RTOG 0232 is a phase III, multi-institutional trial conducted at 68 cancer centers throughout the United States and Canada from 2003 to 2012 to assess whether adding EBT to transperineal interstitial permanent brachytherapy conveyed an additional benefit in progression-free survival (PFS), or control of the cancer growth, at five years following treatment.
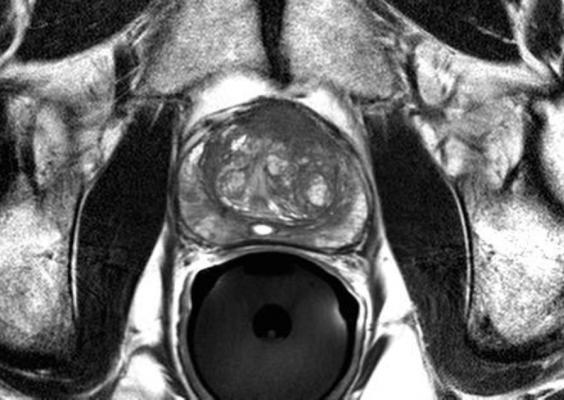
Brachytherapy is a type of radiation therapy (RT) where radioactive seed implants are inserted directly into a patient’s tissue to deliver treatment to the tumor while limiting radiation exposure for surrounding tissue.
Participants in the study included 588 men diagnosed with intermediate-risk prostate cancer (i.e., clinical stage T1c-T2b) and enrolled in the trial between 2003 and 2012. Prostate cancer risk groups are assigned based on the prostate biopsy results, which include the Gleason score (GS) — an indication of how aggressively the tumor cells may behave — and the prostate-specific antigen (PSA) level in the patient’s blood at the time of diagnosis. Eligible patients for this trial had either a GS between two and six coupled with a PSA between 10 and 20; or a GS of 7 and a PSA less than 10.
Patients were randomized to one of two treatment arms, where 292 patients received brachytherapy alone (the B group) and 287 patients received 45 Gy partial EBT to the pelvic area in addition to brachytherapy (the EBT+B group). Brachytherapy treatment included the use of I-125 or Pd-103 (radioactive Iodine-125 or Palladium-103), prescribed to 110 Gy or 100 Gy respective boost dose for the patients who received brachytherapy plus EBT, and 145 Gy or 125 Gy respective dose for the patients who received brachytherapy alone. EBT was delivered by either intensity-modulated RT or three-dimensional conventional RT.
The primary outcome for this study, PFS, was estimated using the Kaplan-Meier method, and researchers compared the two treatment arms with two-sample binomial testing. Short-term/acute and long-term/late side effects also were measured, including both gastrointestinal (GI) and genitourinary (GU) toxicities. Treatment groups did not differ significantly on any baseline characteristics. The median participant age was 67, two-thirds of patients (67 percent) had stage T1 disease, and 89 percent fell in the GS 7/PSA < 10 group. Median follow-up for all patients was 6.7 years, and 443 patients were eligible for five-year follow-up analyses.
At five years following RT, survival rates for men who received brachytherapy alone were comparable to those who underwent more aggressive radiation treatment. The PFS rate at five years post- treatment was 85 percent for EBT+B patients and 86 percent for B patients (Hazard Ratio, HR, 1.02; futility p = 0.0006).
Although PFS rates were comparable between treatment groups, differences emerged in the rates of more serious side effects. Overall toxicity levels were similar across groups only for acute side effects (i.e., those that occur closely following treatment), with eight percent of patients in each cohort reporting acute grade 3+ side effects. Late severe toxicities were more common for EBT+B patients (12 percent) than for B patients (7 percent), as were severe GU side effects GU (7 vs. 3 percent) and severe GI toxicities (3 vs. 2 percent).
“These findings suggest that many men with intermediate-risk prostate cancer can be well managed with seed implant alone and do not require the addition of external beam radiation,” said Bradley Prestidge, M.D., lead author of the study and medical director of the Bon Secours Cancer Institute at DePaul Medical Center in Norfolk, Va. “Contrary to expectations, the more aggressive, combined treatment did not result in superior cancer control rates at five years follow-up, indicating that men can achieve a similar survival benefit with fewer late side effects through brachytherapy alone.”
For more information: www.astro.org


 April 10, 2024
April 10, 2024