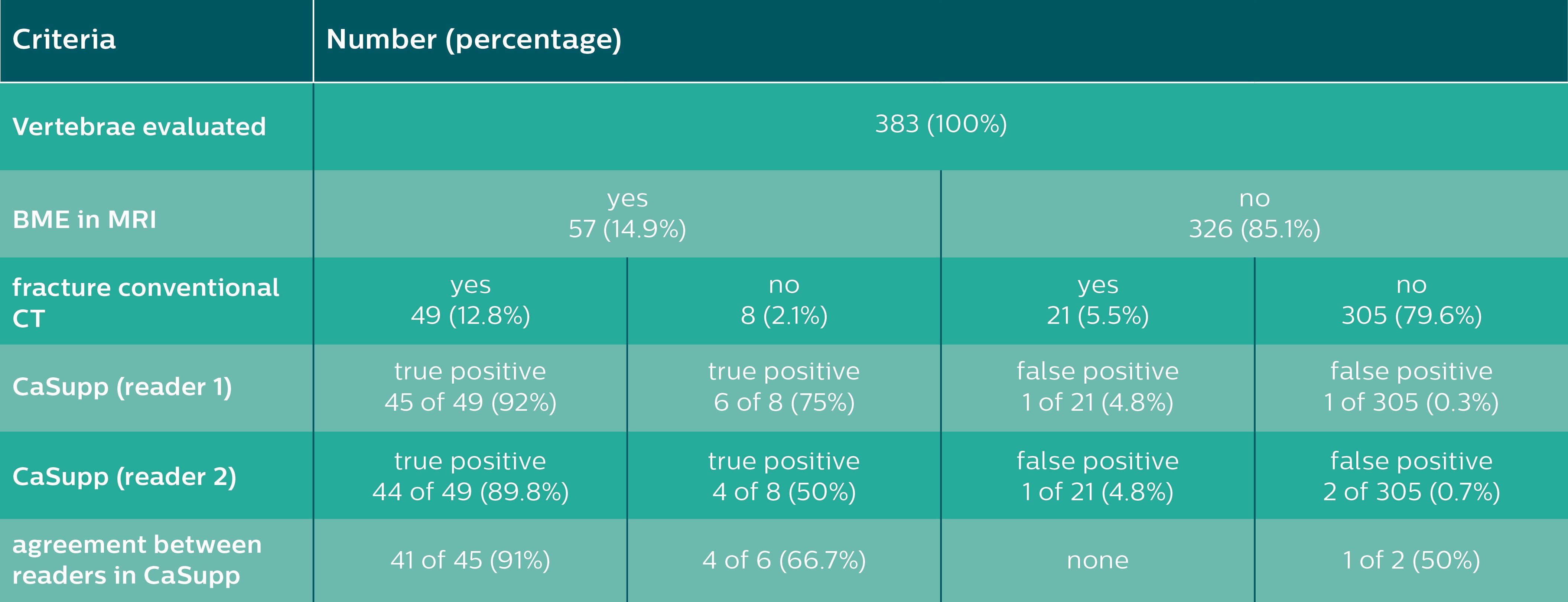
Results of the vertebrae-based analysis (383 vertebrae in 34 patients) for detection of BME.
The following is a summary of a study published in the European Journal of Radiology, 105 (2018) 216–220, by Victor Neuhaus, M.D., and colleagues from the University Hospital of Cologne, Cologne, Germany
The purpose of the study was to evaluate the use of calcium suppression images (CaSupp) provided by Philips IQon Elite Spectral CT to enhance the diagnostic accuracy of detecting bone marrow edema (BME) in vertebral fractures (VF).
Overview
Vertebral fractures are common and require individual treatment, as they are associated with considerable morbidity, mortality and future fractures. Therefore, a precise diagnostic workup of vertebral fractures is crucial for adequate clinical management.
In clinical routine, X-ray and CT of the spine are performed as the initial assessment of VF. However, the dense trabecular bone can obscure the visualization of post-traumatic bone marrow changes, making MRI the modality of choice to differentiate acute and chronic VF based on the presence or absence of BME. But one of the limitations of using an MRI for this assessment is an MRI’s limitation in helping the clinician adequately visualize trabecular and cortical bone structures. This means that assessing both high contrast (trabecular bone) and low contrast tissues (bone marrow) in one examination can be a challenge.
To address this issue, IQon Elite Spectral CT introduced a CaSupp image to its list of spectral results available for every patient scanned on an IQon Elite. With these images, voxels containing calcium are suppressed and replaced by virtual HU values, as similar as possible to the expected HU, without the calcium contribution to the attenuation. The extent of calcium suppression can be modified using different calcium suppression indices. Bone marrow changes, normally obscured by the dense trabecular bone, may be visualized and therefore allow for the detection of traumatic BME.
Methods
This study involved a retrospective analysis of 34 patients, scanned on the IQon Elite Spectral CT, a dual-layer spectral detector CT (SDCT). All of these patients were diagnosed with at least one vertebral fracture and had undergone a complementary MRI. The MRI images were evaluated in order to detect vertebrae with traumatic BME.
Two readers, who were blinded to the results of MRI, evaluated CaSupp for vertebral BME and determined the optimal calcium suppression indices for visualization of BME. In addition, bone mineral density was assessed based on ROI measurements. Moreover, one reader measured the attenuation and standard deviation of BME in fractured and normal vertebrae previously determined in MRI using ROIs in the CaSupp images. The measurements were conducted at different CaSupp indices, ranging from 30 to 100 with an increment of 10 in order to calculate contrast-to-noise ratios.
For the results of the detection of BME, specificity, sensitivity, positive and negative predictive value, and accuracy were calculated. Statistical tests were performed for interrater agreement and contrast-to-noise (CNR) analysis.
Results
A total of 383 vertebrae were assessed in 34 patients. MRI revealed BME in 57 out of 383 vertebrae (14.9 percent). Of the 57 vertebrae showing BME in MRI, both readers detected 51 and 48 true positive vertebrae with BME in CaSupp, respectively. In contrast to that, two and three false positive findings of BME were reported by Reader one and Reader two (see Table 1).
Overall, CaSupp yielded an average sensitivity of 87 percent and specificity of 99 percent, a positive predictive value of 95 percent, a negative predictive value of 98 percent and an accuracy of 97 percent for the detection of fracture-associated edema.
Edema adjacent to the cortical endplates was better visualized using CaSupp index of 70 and 80, while extensive edema (BME extending throughout the trabecular bone compartment) was better visualized using a CaSupp index of 90 and 100 (chi2<0.0001).
No correlation between optimal CaSupp-index and trabecular density was found (p>0.2). CNR of BME increased with higher CaSupp index, with the peak value observed at the highest CaSupp-Index of 100.
Conclusion
CaSupp images reconstructed from IQon Elite Spectral CT allowed the clinician to better visualize and identify BME in traumatic fractured vertebrae with a high diagnostic accuracy using CaSupp indices of 70-100.
The high negative predictive value emphasizes the potential of CaSupp to rule out BME due to acute or subacute fracture. Additionally, CaSupp has shown the potential to assist the clinician in the detection of occult fractures since BME in vertebrae without morphologic signs of fracture in conventional CT were also detected.
Clinical Relevance
CaSupp results available on the IQon Elite Spectral CT can serve as a preset for reconstruction in patients with suspicion of BME.
Citation
Neuhaus, Victor, et al. “Bone Marrow Edema in Traumatic Vertebral Compression Fractures: Diagnostic Accuracy of Dual-Layer Detector CT Using Calcium Suppressed Images.” European Journal of Radiology, vol. 105, 2018, pp. 216–220., doi:10.1016/j.ejrad.2018.06.009.
Disclaimer: Results from case studies are not predictive of results in other cases. Results in other cases may vary.
Philips reserves the right to make changes in specifications and/or to discontinue any product at any time without notice or obligation and will not be liable for any consequences resulting from the use of this publication.


 April 13, 2024
April 13, 2024