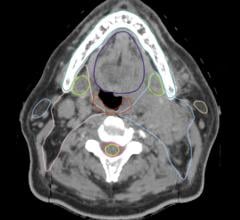
Photo courtesy of Philips Healthcare
Picture, for a moment, the following: You are making acquaintance with someone new who is not in the medical profession, and the first question they ask you is What type of physician are you? or, What is your specialty? You pause for a moment, trying to decide how best to describe your specialty, aware that the answer to this question may necessitate a long-winded follow-up explanation. You are well-seasoned with the array of questions which may ensue — Do you treat with radiation? Do you do nano-surgery? What part of the body do you deal with? Even if their frame of reference is within the medical profession itself, it is unlikely your audience has ever ventured into the depths of the radiology department to see the going-ons in the angio suite, the complex and ever-expanding tools in your arsenal for treating everything from cancer to trauma to varicose veins. If one’s daily routine is anything like the author’s, this uncomfortable experience has replayed itself almost weekly for the last several years — how do you explain to the layperson what interventional radiology is?
Interventional Still Missing From Headlines
In 2017, a high-profile and shocking event made international news — a U.S. Congressman was shot during a Congressional baseball game for charity and sustained life-threatening injuries. Many readers are likely aware that, if not for the emergent pelvic embolization procedure performed by an interventional radiologist, a procedure habitual to many of us, this congressman may not have survived. More recently, in May 2018, the First Lady of the United States, Melania Trump, underwent an embolization procedure for a “benign kidney condition,” according to the statement released by the White House.1 And yet, perusing the national media outlets in the days and weeks after both of these incidents, one would be hard-pressed to find the terms interventional radiologist, interventional radiology or even radiologist when acknowledging the critical procedures performed and the physician who performed them.
In a detailed account of the representative’s care, one source described “surgeries” as part of his treatment but did not acknowledge interventional radiology or even interview the radiologist who performed the embolization procedure.2, 3 When asked to describe his recovery, the representative was quoted as stating he had undergone “many surgeries” without referring specifically to an interventional radiologist.2 The First Lady’s embolization received similar treatment by the national press, with one of the major media outlets even interviewing a urologist and not a radiologist about her procedure;4 to this day, one would be hard-pressed to find IR mentioned in the press as part of her therapy.
Why does interventional radiology as a specialty not receive the same appreciation among the general public or media outlets akin to the same awareness and prestige that other specialties like cardiology and vascular surgery do? One reason is that the terms intervention or interventionalist do not have the same intimacy nor connotate the same level of expertise that such terms as operation or surgeon do. According to the Merriam-Webster dictionary, to intervene is “to interfere with the outcome or course especially of a condition or process (as to prevent harm or improve functioning)” — this is quite vague and does not describe the reality of performing an intricate hands-on medical procedure that requires years of training to master.
Synonymous words for intervention are nondescript and include intercede, intermediate and interpose. For the majority of human beings who are not familiar with the daily workings of a hospital, it is conceivable to lump the terms interventional and radiologist and believe that an interventional radiologist literally intervenes on the amount of radiation delivered to a patient, such as a radiation oncologist does, rather than perform a complex life-saving procedure akin to surgery using imaging as guidance. The second reason is more simple — monikers such as cardiologist, pulmonologist, cardiac surgeon and vascular surgeon are well recognized and respected by the general public in part because these titles denote a physician who is an expert in a specific organ system — heart, blood vessels, lungs, etc. The interventional radiologist does not have ownership of any specific organ system, but rather a technology, a.k.a. radiology.
Educate the Public
“So what?” one might ask. “Why does it matter if IR is recognized by the general public or the media?” Isn’t it sufficient that those in the upper echelons of clinical practice are well familiar with what we do as a specialty? The answer is not so simple. As much of medical practice has trended toward close administrative oversight, it is a cause of concern if the nuances and intricacies of IR may be lost on hospital administrators with limited clinical background, or a mystery to patients who are more and more quizzical of medical professionals.
This specialty’s growth and ultimate survival may become more and more dependent on educating hospital administrators and the general public to become well-versed in the important procedures that IR perform and their critical value to clinical care. Branding a specialty with a title that is not abundantly coherent to a target population, therefore, limits the ability to grow the specialty and compete with those with more well-defined niches. So, cardiologists and vascular surgeons may always get priority over IRs in vascular disease because their brand qualifies them as specialists of these diseases; so, too, radiation oncologists will always have an oncology referral base, while the IR community will struggle to educate administrators and patients about the important role IR plays in cancer therapy. The referring physicians we depend on may even have a gap in understanding of IR — there is evidence that, at least up until recently, many medical students were unfamiliar with IR as a specialty and what exactly an IR does.5
Time to Re-brand
Why, then, adhere to a title that is vague, confusing and ties your specialty to a technology (radiology) as opposed to a part of the human body, and whose description is vague (intervene) as opposed to defined by an advanced skill set?
It is time for IR to consider the possibility of re-branding and marketing itself for what it is — a community of specialists who perform cutting-edge operative therapies for multiple diseases throughout the human body. Consider, for example, the different accolade or recognition we would command among the general public, the media or hospital administrators if we referred to ourselves as radiologic surgeons or surgical radiologists? Or consider the window of opportunity presented by the advent of the IR residency pathway for this specialty to completely detach from the guild of radiology and instead refer to itself as, say, minimally invasive surgery or image-guided surgery?
We should reflect on and be proud of the remarkable skill set it takes to recanalize an occluded vessel, salvage a bleeding organ after a gunshot wound or direct chemotherapy to an isolated focus in the liver, and deserve fair recognition for these achievements. It is time we advertise ourselves proudly and firmly as leaders in delivery of healthcare, not service providers that take a backseat in the public eye to surgeons. Perhaps a call to action is upon us to find another, more recognizable and encompassing term we can ascribe to our specialty that more creatively captures the delicate and critical procedures we do, so that we are recognized as leaders in delivery of care and not followers behind other specialties.
References:
1 Statement from the Communications Director about First Lady Melania Trump. (2018, May 14) Retrieved from https://www.whitehouse.gov/briefings-statements/statement-communications-director-first-lady-melania-trump/ Accessed Dec. 17, 2018.
2 Stolberg S.G. Three Months After Shooting, Steve Scalise Makes Emotional Return to House. (2017, Sept 28) https://www.nytimes.com/2017/09/28/us/politics/steve-scalise-return-house-shooting-baseball.html Accessed Dec. 17, 2018.
3 Kolata G. Scalise Faces Prospect of Multiple Operations. (2017, June 15) Retrieved from https://www.nytimes.com/2017/06/15/science/steve-scalise-shooting.html Accessed Dec. 17, 2018.
4 Scutti S. Melania Trump’s Kidney Procedure Explained. (2018, May 15) Retrieved from https://www.cnn.com/2018/05/14/health/melania-trumps-kidney-procedure-explained/index.html Accessed Dec. 17, 2018.
5 Nissim L, Krupinski E, Hunter T, Taljanovic M. Exposure to, understanding of, and interest in interventional radiology in American medical students. Acad Radiol. 2013 Apr;20(4):493-9.
Lavi Nissim, M.D., is a board-certified interventional radiologist living in Scottsdale, Ariz. He currently is employed by Envision Healthcare. He is in fellowship training in both adult and pediatric IR and a graduate of the University of Pennsylvania School of Medicine.
Related content:
U.S. First Lady Melania Trump Undergoes Interventional Radiology Embolization Procedure



 April 22, 2024
April 22, 2024