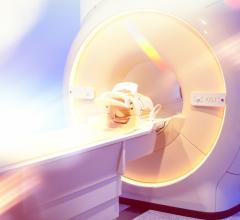
The Elekta Unity with 1.5T MRI embedded as a targeting system appeared at the annual meeting of the American Society of Radiation Oncology (ASTRO) in San Antonio, Texas. The system is being sold in Europe and could soon enter the U.S. marketplace. (Photo courtesy of Elekta)
A linear accelerator combined with high-field MRI could soon be on the U.S. market. If U.S. regulators do as expected, it will be the second such system.
The Swedish vendor Elekta exhibited the U.S. Food and Drug Administration (FDA)-pending system, called Unity, on Oct. 21, the first day of the annual meeting of the American Society of Radiation Oncology (ASTRO) in San Antonio, Texas. It received the CE Mark early last summer, opening the door to sales in Europe. At summer’s end, the Swedish company submitted a 510(k) application about the system to the FDA.
Already on the U.S. market is ViewRay’s MRIdian, which cleared the regulatory agency in February 2017. It, like Elekta’s Unity, use MRI to visualize patients during radiation treatment and adjust the radiation beam to improve targeting.
Unity integrates a 1.5T scanner, an adaptation of the Ingenia diagnostic system from Philips Healthcare. Elekta’s chief marketing and sales officer, Ioannis Panagiotelis, said the image quality allows exceptionally exact targeting.
ViewRay’s MRIdian uses a lower field scanner but features, according to Michael Saracen, ViewRay’s vice president of marketing, a “split magnet design,” which allows radiation to shoot right to the patient.”
Although key elements of the 1.5T magnet in the Elekta Unity “leave spaces” through which the treatment beam can pass, the magnet in Unity is not split, Panagiotelis acknowledged. “To have a homogenous field at 1.5T, you can’t separate these elements too much,” he said.
The beam, therefore, must go through metal, he said. To compensate, the beam starts off as “really strong so that when it reaches the patient, it is strong enough.” This attenuation, ViewRay’s Saracen said, is accompanied by radiation scatter.
The exact targeting — and on-the-fly retargeting — of soft tissue targets allows MRI-based systems to deliver higher radiation doses to target pathologies than standard radiotherapy systems, the two men said. As a result, treatment can be completed in much shorter periods than with conventional linear accelerators.
Saracen explained that a six-week treatment might be collapsed to a week. MRIdian, he said, could increase the radiation dosage in each daily treatment. This exposes tumor tissue to the “same killing amount,” while sparing the surrounding tissues. “So by increasing the dose, you can shorten the time to essentially five treatments,” he said.
A Dynamic Market
Entry of a second system into the U.S. market could validate the underlying concept of embedding MRI in radiation therapy machines, potentially driving interest in this still fledgling field. The market, Saracen contended, is already approaching a “tipping point.”
“We are now getting data that this is really making a difference,” he said. “When you can adjust for size, shape and position of the tumor and the surrounding organs at risk — and only deliver dose to where you intend to — you start to see that you can improve outcomes.”
Sites using MRIdian are reporting “compelling” results, Saracen said. Patient survival is increasing, even among very difficult-to-treat patients. Length of survival after initial diagnosis of pancreatic cancer, for example, has gone from 12 months to more than 18, he said. Meanwhile severe complications from radiation toxicity have been reduced. “And we did this while increasing the dose,” Saracen said. “The only way you can do that is if you know exactly what you are treating — and adjust the beam throughout treatment.”
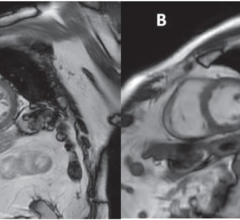
Early results from European sites operating Elekta Unity indicate similar success. Panagiotelis described a patient who received treatment for the recurrence of prostate cancer. This patient — the first treated at the University Medical Center (UMC) Utrecht on its Elekta Unity — was especially challenging, because the patient had been treated conventionally some 10 years earlier. Rising levels of prostate specific antigen led to the discovery of recurrence in a pelvic lymph node.
Utilizing high-field MRI, Elekta Unity was able to visualize the small soft tissue targets before and during treatment, adapting the radiation beam in real time so as to spare the surrounding tissue while administering high doses to the cancer. Five fractions of 7Gy were given over 10 days as part of stereotactic intensity-modulated radiation therapy. Unity’s 1.5 T MR imaging system visualized the treatment area before and during each fraction, then verified the targeted delivery positions. Even with MRI at 1.5T, these targets — which ranged from 2mm to 3 mm — were difficult to visualize, Panagiotelis noted.
Precision Medicine
Saracen said the ability to adjust treatment plans on the fly exemplifies “personalized medicine.” Panagiotelis took the idea a step further, stating that Unity provides “personalized precision cancer therapy.”
Over the course of therapy, the shapes and positions of tumors change, as the radiation sculpts the tumors. This, in turn, affects the shapes and positions of surrounding healthy tissues. MRI-guided radiation therapy can make necessary adjustments.
Detecting changes and adapting therapy could lead to success against some of the most difficult-to-treat cancers, including those of the lung and pancreas, Panagiotelis said.
“Unity characterizes our strategy for the products we are developing today and the ones we are hoping to develop in the future,” he said.


 April 24, 2024
April 24, 2024