Siemens is developing the Magnetom Trio PET/MRI system. The product is under development and not commercially available in the U.S., and its future availability cannot be ensured. The images above show a patient with a neoplasm.
In scientific research, sometimes simply connecting two points with a line is enough to paint the big picture.
When researchers first identified the biomarker amyloid beta-protein for Alzheimer’s disease by using positron emission tomography (PET) imaging, they gained a new perspective on how to treat the disease.
But for this Alzheimer’s biomarker, its fingerprint is only as good as the imaging modality used to detect it.
Hybrid Imaging
In an effort to improve disease detection, researchers connected the two most sensitive imaging modalities for detecting disease — PET and magnetic resonance imaging (MRI).
The combined PET/MRI system is the next frontier in hybrid imaging. This hybrid system delivers specific molecular information related to cell surface reactors, enzymes and gene expression that PET provides. Simultaneously, it also captures important anatomical data, soft-tissue contrast and information about perfusion and permeability shown in MRI.
Preclinical Evidence
Preclinical tests have shown how the new hybrid system can greatly improve imaging capabilities and promises to advance research in many areas.
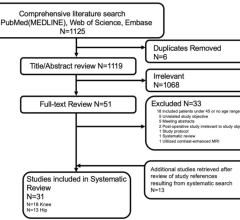
In a study1 conducted at Osaka University Graduate School of Medicine and Medical Hospital, Osaka, Japan, researchers used an integrated PET/MRI system to acquire whole-body images of rats and other small animals.
“Our system shows great promise because it is able to simultaneously provide the complementary strengths of PET and MRI in imaging rats and small animals,” said Mitsuaki Tatsumi, associate professor of radiology at the school.
He added, “This ability opens up exciting new opportunities in research in terms of increased understanding of kinetics, biodistribution of radiopharmaceuticals and, eventually, disease characteristics and physiological processes. Next steps include imaging body tumors in rats or mice and developing PET/MRI systems that can image people.”
Making the Connection
Making the connection between PET and MRI has been a challenge because of interferences that create artifacts or image degradation.
According to an article published online by the Journal of Nuclear Medicine Technology (JNMT) 2, citing a lecture given by Uwe Pietrzyk3, “PET scanners are highly sensitive to magnetic fields and contain conducting and radiofrequency radiating components that have the potential to interfere with the MRI system.”
“Furthermore, the static main magnetic field of MRI prevents the use of classic photomultiplier tubes for radiation detection in PET. Consequently, the design of the PET components has to be fundamentally changed in order to merge the PET and MRI modalities into a single imaging system,” the article said.
When Siemens Medical Solutions married a PET insert to its Trio 3-T MRI head scanner4, it helped push the PET/MRI technologic development into the realm of human research settings.
“The MR-compatible PET detector ring was constructed to fit inside a standard clinical 3-T MR imager to match the two fields-of-view (FOVs). Furthermore, a standard birdcage transmit/receive head coil (Siemens Medical Solutions) mounted on the MR imager bed could be placed inside the PET detector ring, thereby matching the two FOVs. This also enabled temporal and spatial registration of PET and MRI data,” the JNMT article notes.
Today, prototypes are being installed in major U.S. and European institutions with the possible extension to clinical whole-body PET/MRI in the future.
Modality of Choice?
Today, some scientists believe PET/MRI could become the technology of choice in the future.
“Clear synergy exists between PET and MRI, because each can provide unique information not attainable with the other,” state the authors of the JNMT article. One of them, George Remo, Ph.D., assistant professor, nuclear medicine technology baccalaureate program, department of clinical and diagnostic sciences, University of Alabama at Birmingham, believes the new hybrid would most likely be adopted first for the diagnosis of neurological diseases.
“It’s very likely that PET/MRI would start to be used in neurologic investigations, given the fact that both PET and MRI are strong in yielding functional information at the molecular level of neurotransmitters, neuroreceptors, glial biochemistry and electrophysiology. This can have unparalleled implications in brain research and diagnosis when compared with today’s fusion technology,” he said.
It would primarily be used for diagnosing diseases like Alzheimer’s and Parkinson’s disease, Remo adds. Huntington’s disease and amyotrophic lateral sclerosis (ALS) would also benefit from PET’s functionality and MRI’s soft-tissue contrast resolution, functional and spectroscopic abilities.
“Neuropsychiatric disease management in depression, epilepsy and schizophrenia are all going to benefit from the adoption of this new fusion technology,” he said.
But where Remo foresees the biggest benefit is in molecular imaging using biomarkers.
“At the molecular level, the ability of PET/MRI to capture, correlate and document biochemical signatures is unparalleled with any other fusion modality available today,” he said.
Cardiac Imaging
Another potentially major application of PET/MRI is in the field of cardiology.
In particular, PET/MRI could enhance the detection of molecular markers for atherosclerotic plaques and the evaluation of angiogenic or stem cell therapies for diseased cardiac tissue.
“PET/MRI’s ability in assessing flow, diffusion, perfusion and cardiac motion in a single examination coupled with its ability to detect myocardial viability (PET) and metabolism (MRI) can impact coronary disease diagnosis,” Remo said. “It can also help management in a more cost-effective and patient-friendly manner by cutting down intermediaries.”
Remaining Obstacles
In order for PET/MRI to become the technology of choice, it may need to replace dedicated PET/CT, prevalent in the oncology setting. It also would have to justify substituting a dedicated MRI system.
“As with the ubiquitous adoption of any technology, PET/MRI’s acceptance into routine clinical practice would greatly depend upon the price tag associated with acquiring, operating and maintaining this technology in the clinics,” noted Remo. “Also of equal importance, if not greater, will be the future reimbursement levels for PET/MRI studies, which can be a major factor in determining its future ubiquitous deployment and use in the clinics.”
One area in which PET/MRI has a distinct advantage over PET/CT is lower radiation exposure for patients.
“Combining PET with MRI may be a natural answer to the current licensing dilemma facing hybrid technologists operating two seemingly immiscible modalities like PET and CT, each of which currently has modality-specific licensing requirements owing to differences in the nature of ionizing radiation used,” Remo said. He also emphasized the importance of cross-training and education for hybrid technologists who work with PET/MRI. Without such training, the technology might not be adopted. “If PET/MRI can overcome the said challenges, then — owing to its ability to obtain superior anatomic and functional information — it will be on its merry way to becoming the technology of choice of the future,” Remo concluded.
References:
1. Tatsumi M. “Simultaneous C-11 Methionine PET and contrast-enhanced MRI rat imaging with an integrated PET/MRI system.” Scientific Paper: Department of Radiology, Osaka University Graduate School of Medicine and Medical Hospital, Osaka, Japan, SNM’s 56th Annual Meeting, June 13–17, 2009.
2. Bolus N, Remo G, et al. “PET/MRI: The Blended-Modality Choice of the Future?” Journal of Nuclear Medicine Technology Vol. 37, No. 2, 63-71. May 15, 2009.
3. Pietrzyk U. “Recent aspects of hybrid imaging.” Lecture presented at Centre de Physique des Particules de Marseille; Oct. 27–28, 2008, Marseille, France.
4. Burbar Z, Grazioso RF, Corbeil J, et al. “PET performance of MR/PET brain insert tomograph.” In: “Proceedings of the IEEE Nuclear Science Symposium and Medical Imaging Conference.” Piscataway, N.J.: IEEE; 2006.


 April 17, 2024
April 17, 2024