IBM and The Mayo Clinic's BC-10 MRI Coils
The need for orthopedic care in the U.S. has grown considerably in recent years, due in large part to an aging population and an almost obsessive, albeit well-intentioned, preoccupation with physical fitness. Orthopedics now includes subspecialties, such as joint replacement and sports medicine, terms that 30 years ago may have solicited a quizzical “huh?” from the average citizen. But today, almost everyone knows someone who has had knee or hip replacement, and thanks to their man-made prostheses, scores of recipients are once again enjoying life’s most simple pleasures. Similarly, sports-related injuries are no longer confined to professional athletes; increasing numbers of weekend warriors, young adults and even children are hobbling into hospital emergency departments. Add osteoporosis-related injuries, orthopedic complications from auto-immune disorders such as rheumatoid arthritis and lupus, as well as congenital defects, and the result is a plethora of musculoskeletal disorders affecting all ages of the population.
Musculoskeletal disorders are on the rise not only in the U.S., but globally as well. The American Academy of Orthopaedic Surgeons (AAOS) estimates that over half of all chronic conditions in the elderly can be attributed to joint diseases. Recognizing the burden this places on society and healthcare, 50 nations from around the world have designated the 10-year span from 2000 to 2010 as the Bone and Joint Decade. Likewise, President Bush named 2002 to 2011 the National Bone and Joint Decade in the U.S., the goals of which are to increase awareness, empower patients, increase global funding for prevention and research, and seek and promote cost-effective prevention and treatment of musculoskeletal injuries and disorders.
Driven in part by this increased awareness — including better-informed patients — the tools and techniques used to diagnose and treat orthopedic conditions are evolving. According to a recent study released by Frost & Sullivan, the market is concentrating on products and solutions that produce greater efficiency, ease of use as well as economic advantages. Orthopedic imaging is leveraging MRI, PACS and image-guided tools to improve diagnosis, planning and navigation through surgery.
Better Diagnostics for Better Outcomes
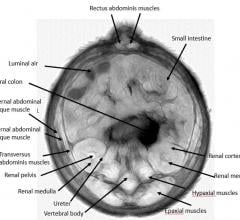
One technology garnering much attention in orthopedic circles is magnetic resonance imaging (MRI), which for the purposes of orthopedic imaging can include whole-body scanners, extremity-specific coils and extremity-dedicated units. These devices allow physicians to view in detail cartilage, tendons and ligaments as well as bony structure.
The Mayo Clinic has developed, in collaboration with IBM Engineering and Technology Services, BC-10 MRI Coils, which are used specifically to image the fingers, wrist, forearm and elbow. According to Joe Nemeth, VP of Medical, IBM Engineering and Technology Services, IBM engineers worked with Mayo’s laboratory prototype, which was based on years of medical research, and redesigned the electrical components, tweaked the coils’ ergonomics and optimized overall functionality for the benefit of both the technician and the patient. The result is very robust, miniature coils, available in both 1.5T and 3T, that are highly sophisticated in design and produce high-resolution, detailed images that aid in the diagnosis of arm and hand injuries and disease.
“The level of detail and resolution we are now obtaining has allowed for more definitive diagnosis based upon imaging — something we have been previously cautious about stating,” said Richard Berger, M.D., Ph.D., orthopedic surgeon at Mayo Clinic.
Kimberly Amrami, M.D., a Mayo Clinic radiologist, added, “Accurate diagnosis is the critical forerunner to effective medical treatment, which is why Mayo focused on improving the diagnostic capabilities of magnetic imaging.”
The OrthOne Dedicated High-Field MRI Extremity System from ONI Medical, which is said to rival the quality of whole-body systems, is a small-footprint unit that American Radiology Service Inc.’s Timonium Crossing facility finds ideal for small parts imaging. “In MR imaging, the smaller the coil and the closer you image to the body part, the better signal to noise [ratio] you receive. The same goes for the sweet spot — if the sweet spot is smaller, then it just makes sense that you get a better image,“ explained Robert Evers, clinical director of MRI, American Radiology Service Inc. “In a whole-body scanner, because you have to evaluate a large field of view, the sweet spot is much larger and therefore images can drift.”
MRI not only plays an important role in orthopedic imaging as a diagnostic tool, but also as a measure of the prognosis of orthopedic disease. Last November, GE Healthcare sponsored a Webinar entitled The Future of Imaging in Orthopedics, in which presenter, Hollis G. Potter, M.D., stressed the importance of MRI in predicting the success of a surgery. Potter, who is chief, Magnetic Resonance Imaging, Hospital for Special Surgery, professor of Radiology, Weill Medical College of Cornell University, indicated that MRI allows for the quantification and precise localization of particle disease, and that it can detect compression of adjacent nerves and vessels. In the future, Potter believes, MRI will be helpful in the serial evaluation of painful arthroplasty and allowing for detection of the joint lining at the origin of the biologic reaction.
PACS in the OR
When their job brings them into the OR, orthopedic surgeons today have a legion of tools at their disposal to aid in surgical planning and execution. For instance, no longer confined to the relatively simple task of displaying and storing images, PACS has matured and moved beyond radiology to other areas within the hospital, including the OR. For the orthopedic surgeon, this means that patient images needed to digitally plan surgeries are just a mouse-click away.
One such solution aiding surgeons is OrthopedicPACS, which combines TraumaCad (Orthocrat Ltd.) planning software with NovaRad’s NovaPACS software and imaging accessories, integrating patented Ortho tools with a NovaPACS workstation. TraumaCad enables advanced orthopedic surgical planning through precise manipulation of soft-copy images and application of fixation and prosthetic systems. It also includes advanced modular deformity correction and pediatric packages.
TraumaCad is also available as part of the Fuji Synapse PACS offering, as a result of a recent agreement between Orthocrat and FUJIFILM Medical Systems USA. Now physicians simply log in to the integrated solution, access patient images through the PACS and drag and drop them into the TraumaCad workspace. Completed surgical plans are then saved to the Synapse archive along with other patient files.
Making its recent debut at the 2006 AAOS Annual Meeting, the Cedara OrthoWorks ProPlanner is a soon-to-be-released workstation or customizable plug-in clinical application for orthopedic support designed for use on existing PACS and RIS/PACS systems.
Extending beyond basic orthopedic planning, OrthoWorks ProPlanner provides support for deformity corrections, trauma and customized planning methodologies that mimic orthopedic workflow. In challenging deformity and trauma corrective cases, for example, image cutting allows surgeons to cut and reposition fractured bone fragments to visualize potential surgical changes. In converse circumstances, Image stitching allows users to stitch together two or more images using a number of methods to ensure that cases requiring long film X-rays can still be digitally planned without the need for expensive stitching hardware. OrthoWorks ProPlanner also incorporates Cedara’s unique ImageSnap Technology that enables automatic measurements with suggested implant selection and placement.
Computer-Assisted Surgery
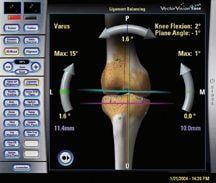
Another information technology solution finding its way into the orthopedic surgical suite is computer-assisted surgery. Michael L. Swank, M.D., director of the Joint Replacement Center at Jewish Hospital, Cincinnati and chairman of the board, Freiberg Orthopedics & Sports Medicine, likens use of these systems in the OR to using a GPS versus a map when driving. “If you use a GPS, you plan out your route, and when you are driving along, it tells you exactly where you are relative to where you want to be. You don’t have to make a judgment about it; [the GPS] provides you, if you will, with that judgment. The use of computers in the OR is pretty much used the same way.”
A pioneer in the use of computers for orthopedic surgery, Swank has spent several years researching and performing clinical trials with BrainLab’s VectorVision image-guided navigation system. In joint reconstruction surgeries, precise positioning and implant alignment are crucial components of a procedure’s success. The VectorVision allows for smaller incisions, more precise cuts, balancing soft tissue, individualized patient plans and elimination of long rods for bone alignment, which, as clinically documented, all add up to less pain, faster recoveries and better patient outcomes.
To use the system, the surgeon places small trackers on the bones to map out the patient’s anatomy. Based on that information, the computer generates a surgical plan to ensure the patient’s bones are in the proper position and the implants are properly placed, including a 3-D map of the bone, a plan on how to cut the bone and what size implant to use.
“Image-guided navigation technology for orthopedic surgery is designed to allow a surgeon to align an artificial joint with greater precision within the body,” said Dr. Paul Di Cesare, chief of Adult Reconstructive Surgery, NYU Hospital for Joint Diseases. The facility recently installed Stryker’s surgical navigation system for hip and knee joint replacement surgeries. “Precise alignment is an important factor that may reduce joint wear and extend the life of the implant. Use of the system has many potential benefits including improved joint stability and range of motion,” Dr. Di Cesare explained.
Currently, only about 10 percent of all joint replacement surgeries utilize computer assistance. In about five years, says Dr. Swank, once the more experienced surgeons — who perform the lion’s share of replacement surgeries — adopt the technology, and the younger surgeons who have been trained on it prove themselves, computer-assisted systems will be the standard of care for orthopedic surgeries.
Technology Paves Way for the Future
As innovative technology paves the way for the future of orthopedic care, Potter emphasizes the importance of imaging’s evolution in orthopedics. “Imaging technology drives implementation of new outcome assessment, allowing for earlier detection of disease,” said Potter, “and also allows us to noninvasively monitor progression of disease and more comprehensively allow us to assess our ability to intervene and modify these processes and, hopefully, slow the rate of disease progression.”




 April 28, 2020
April 28, 2020