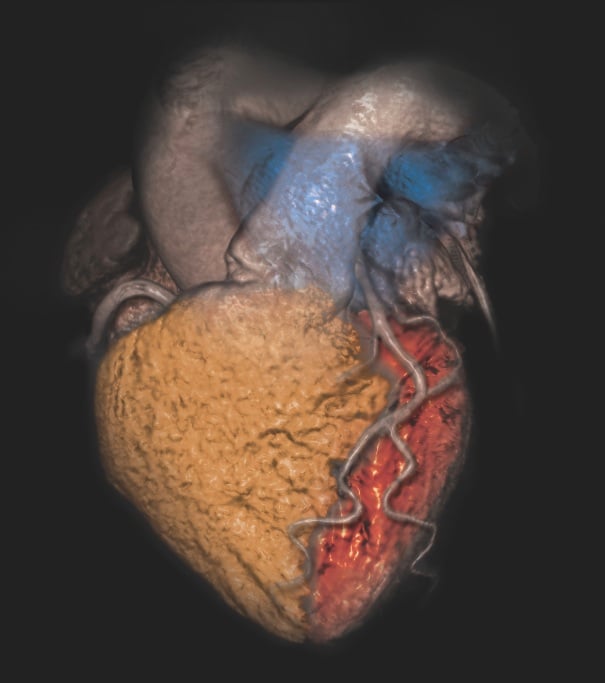
February 28, 2014 — Determining the appropriate use of cardiovascular imaging requires analyzing the “complex interplay” among care processes and their quality, patient health outcomes and medical costs, according to a health policy statement released by the American College of Cardiology (ACC) and endorsed by 14 other relevant medical societies.
The document discusses the current understanding about the patterns and drivers of imaging use, along with patient safety and test quality. It notes that a more patient-centric approach to guiding appropriate use is needed than payer-driven reimbursement reductions and prior authorization requirements.
Drafted by a writing committee of physicians, administrators and consumers, the statement acknowledges the dramatic increase in imaging that began in the late 1990s, which fueled concern that use was driven by an unregulated fee-for-service reimbursement system. However, the document also cites evidence of a recent drop in utilization and shows that multiple factors affect physician test ordering, including greater patient demand and defensive medicine.
Recognizing the important different perspectives that converge in health policy, the statement warns that “simplistic causal models” connecting reimbursement with utilization can lead to bad policy that may harm patients. As examples, the document notes that prior authorization policies may seriously limit patient access to care services. Reducing reimbursement for office-based care as a way to lower costs can, and has, led to unintended shifts to more expensive hospital-based care.
As an alternative, the statement advocates a more sophisticated approach to shepherding responsible imaging use. It suggests that imaging policy could benefit from “an iterative process” using “relevant, high-quality data to guide continued efforts.”
“The current situation in non-invasive cardiovascular imaging is pretty much unsatisfactory from everyone’s point of view,” said Daniel B. Mark, professor of medicine at Duke University School of Medicine, director of outcomes research at the Duke Clinical Research Institute, and the chair of the statement’s writing group. “However, it is encouraging that we now have much more knowledge and several new informatics tools that can be used to help us apply that knowledge. We have many of the ingredients needed to create a more responsible, cost-conscious approach to imaging that still preserves — at its core — patient-physician decision making.”
Both randomized trials and clinical registries could be used to provide the needed information on patient outcomes, resource use and medical costs, the statement suggests. In addition, electronic medical records could promote the efficient use of point-of-care tools, such as appropriate use criteria and decision support systems. These resources would combine patient-specific information with statistical models and other prediction rules.
The statement moreover identifies the role physician groups play in promoting appropriate imaging use. For example, the ACC’s FOCUS program pairs local chapters with health plans to reduce geographic variation in imaging use and lower the rate of “rarely appropriate” tests. Additionally, the American Medical Association is working to define performance measures that include the quality and appropriate use of cardiovascular imaging.
“The complexity of our current health care system and the competing macro-forces that push it in myriad different directions can make responsible imaging use seem impossibly daunting,” Mark said. “What we need is a convergence of will to make it happen from all key stakeholders. This statement hopefully is a step in that direction.”
This statement was endorsed by the American Heart Assn., American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Intersocietal Accreditation Commission, Mended Hearts, North American Society for Cardiovascular Imaging, Radiological Society of North America, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions Foundation, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance and the Society of Nuclear Medicine and Molecular Imaging. Their 2014 Health Policy Statement on Use of Noninvasive Cardiovascular Imaging was published Feb. 25 in Journal of the American College of Cardiology.
For more information: www.cardiosource.org


 April 23, 2024
April 23, 2024