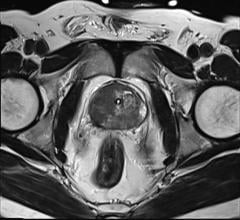
Photo courtesy of Siemens Healthcare
Molecular imaging is a broad and dynamic field that encompasses a range of image technologies that allow physicians and researchers to noninvasively visualize biological processes at the cellular and molecular level. Currently, the vast majority of clinical applications of molecular imaging use radiolabeled compounds (radiopharmaceuticals) that are detected with gamma cameras, single-photon emission computed tomography (SPECT) or positron emission tomography (PET), depending on the type of radioactivity used. Molecular imaging techniques typically complement more anatomic-based imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI), and hybrid imaging modalities including SPECT/CT, PET/CT and more recently PET/MRI are available for clinical use. Together, multimodality molecular imaging can more accurately localize and characterize disease processes than either modality alone.
Here, we briefly highlight several applications of molecular imaging that are poised to have major growth over the next few years. Novel radiopharmaceuticals for prostate cancer imaging, PET agents targeting amyloid for the evaluation of dementia and radiolabeled antibodies for immunoPET are in advanced stages of development. Each of these applications help address relatively common unmet clinical needs not readily answered with anatomic based imaging modalities. In addition to use in clinical care, these radiopharmaceuticals can be used as imaging biomarkers in clinical trials to develop therapeutics.
Prostate Cancer Imaging
Prostate cancer is the most common cancer in men in the United States with the exception of skin cancer. Approximately one in seven men will be diagnosed with prostate cancer in their lifetime, and prostate cancer is the second leading cause of cancer death in men.1 Treatment options for localized prostate cancer include surgery (radical prostatectomy) and external beam radiation therapy, while metastatic prostate cancer is treated with androgen deprivation therapy (ADT) and other systemic therapies. A common clinical scenario in the care of men with prostate cancer is biochemical recurrence after definitive therapy with surgery or radiation detected by serum prostate-specific antigen (PSA) measurement. In these men, it is critical to accurately localize the recurrent prostate cancer in order to provide appropriate therapy, but CT and MRI have low sensitivity for detecting recurrence in this patient population. Skeletal scintigraphy with radiopharmaceuticals such as Tc 99m-MDP and F-18 fluoride are sensitive for detecting bone metastases, but do not evaluate soft tissues including the prostate bed and lymph nodes. The glucose analogue F-18 FDG, which is effective for imaging a wide range of human cancers, has limited utility in prostate cancer until it becomes more advanced. Thus, there is a great need for more accurate methods for detecting and localizing recurrent prostate cancer.
A number of radiopharmaceuticals have been developed that are superior to CT and MRI alone for detecting recurrent prostate cancer.2 C-11 choline, a naturally occurring compound that is incorporated into cell membranes, has received FDA approval for PET imaging in men with suspected prostate cancer recurrence but negative or equivocal conventional imaging.3 Choline-PET/CT appears to be superior to CT or MRI alone for detecting lymph node metastases while MRI is superior for evaluating the prostate cancer bed. One shortcoming of choline-PET is the 20 minute half-life of C-11, which limits batch production and remote distribution. Alternatives to C-11 choline for prostate cancer include F-18 labeled analogues of choline which take advantage of the longer half-life of F-18 (110 minutes), the non-natural amino acid F-18 FACBC which targets upregulated amino acid transport in prostate cancer, and radiolabeled small molecules binding to the prostate-specific membrane antigen (PSMA) which is over expressed on the surface of prostate cancer cells. All of these compounds have shown promising imaging properties in research studies in men with recurrent prostate cancer, and one or more of these tracers may become available in the United States for clinical use.
Amyloid-PET for the Evaluation of Dementia
Alzheimer's disease (AD) is the most common cause of dementia, accounting for approximately 60-80 percent of cases of dementia in the United States. AD currently affects over 5 million Americans and is the sixth leading cause of death.4 Pathologic hallmarks of AD are the deposition of extracellular beta-amyloid protein and intracellular deposition of tau protein accompanied by brain atrophy and neuronal loss. The pathophysiologic process underlying AD proceeds clinical manifestations of cognitive impairment by up to 20 years. Currently, the clinical diagnosis of AD is based on history taking and objective cognitive testing, but atypical presentations and co-morbid illnesses can confound the diagnosis. Additionally, neurodegeneration is advanced at the time of clinical presentation, and earlier detection may be necessary for therapeutics to be effective. FDG-PET can be used to distinguish AD from frontotemporal dementia (FTD) based on regional patterns of decreased FDG uptake, but the specificity of FDG-PET is lower for other types of dementia. The accurate diagnosis of dementia is important for patients and their families for life planning and will become even more important when therapies that slow the progress of AD become clinically available.
Amyloid-PET has emerged as an important imaging biomarker in the assessment of patients with cognitive impairment.5 C-11 labeled Pittsburgh Compound B (PiB) has been widely used in research studies for measuring amyloid levels in the brain. Recently, F-18 labeled radiopharmaceuticals have been developed including the FDA-approved radiopharmaceuticals florbetaben, florbetapir and flutemetamol for the evaluation of patients with cognitive impairment. These PET tracers bind to the fibrillary form of beta-amyloid in the brain, and negative studies make AD very unlikely as the cause of a patient's cognitive impairment. However, negative studies do not exclude other dementias that do not have elevated levels of brain amyloid. Additionally, positive amyloid PET studies can occur in cognitively normal individuals, and amyloid alone does not establish the diagnosis of AD or any other neurological disease. The Society of Nuclear Medicine and Molecular Imaging (SNMMI) and the Alzheimer's Association have published appropriate use criteria for clinical amyloid-PET.6 Despite FDA approval, these amyloid PET tracers have had limited clinical use due to lack of reimbursement by CMS. Recently, a plan for coverage with evidence development (CED) has been approved by CMS to reimburse clinical amyloid-PET scans performed as part of a research study evaluating change in patient management. Although still in the planning stages, this study is expected to begin in early 2016 and will make amyloid-PET more widely available for clinical imaging.
ImmunoPET
The push for personalized and precision medicine has led to the rapid expansion and development of many targeted therapeutics in oncology and other disease states. Treatment with targeted therapeutics can be expensive and associated with toxicity, and the presence of the molecular target assessed by in vitro assays does not always indicate response to therapy. Thus, there is a need for the imaging tools for evaluation of the specific tumor antigens/receptors targeted by these therapies. Imaging agents can overcome some of the limitations based on biopsy-based tests including target heterogeneity and lesions that are inaccessible. In addition, serial imaging can assess the changes in target density over the course of therapy.
Several recent studies using Zr-89 and I-124 radiolabeled antibodies have shown excellent imaging of extracellular receptors in both preclinical and clinical research settings.7-9 Thus immunoPET, PET imaging based on radiolabeled antibodies, is expanding as an important imaging tool in both academic and industry settings. In particular, immunoPET in oncology can help with stratifying patients that may benefit from antibody therapy, monitoring the course of antibody-based therapeutics and paving the way for the next generation of targeted therapeutics. With the development of several antibody drug conjugates (ADCs), antibody-based targeting vehicles with a toxic payload, confirmation and quantitation of drug targeting becomes particularly important.
Human immunoPET studies at several sites have shown the feasibility of using Zr-89 trastuzumab to image HER2 expression in patients with metastatic breast cancer and studies are ongoing to assess how this relates to response to HER2 targeted therapeutics.10, 11 Other studies have shown that the radiolabeled version of the therapeutic VEGF targeted antibody, Zr-89 bevacizumab, can be used to predict response to certain antiangiogenic therapies in certain patient populations.12 The use of radiolabeled versions of new antibodies has also been suggested in order to select patients for clinical trials for these new therapies.13 While more data is needed to fully understand the utility of these agents, these promising studies provide the basis for future work in this area.
Disclosures
Eli Lilly/Avid Radiopharmaceuticals:
consulting, research support
Blue Earth Diagnostics: consulting
Jonathan McConathy, M.D., Ph.D., is assistant professor of radiology at the Mallinckrodt Institute of Radiology, Washington University School of Medicine. He is also president of SNMMI's Center for Molecular Imaging Innovation and Translation (CMIIT) and chair of the society's Brain Imaging Outreach working group.
Suzanne Lapi, Ph.D., is associate professor of radiology and biomedical engineering and director of isotope production at the Mallinckrodt Institute of Radiology, Washington University School of Medicine. She is also vice president of SNMMI's Radiopharmaceutical Sciences Council.
References
1. Prostate Cancer Facts and Figures, 2015. American Cancer Society. www.cancer.org/cancer/prostatecancer/detailedguide/prostate-cancer-key-statistics. Accessed June 2, 2015.
2. Jadvar H. "Molecular imaging of prostate cancer with PET." Journal of Nuclear Medicine: official publication, Society of Nuclear Medicine. 2013;54(10):1685-8. Epub 2013/10/03. doi: 10.2967/jnumed.113.126094. PubMed PMID: 24084704.
3. FDA prescribing information for C-11 choline. www.accessdata.fda.gov/drugsatfda_docs/label/2012/203155s000lbl.pdf. Accessed June 2, 2015.
4. 2015 Alzheimer's Disease Facts and Figures. Alzheimer's Association. www.alz.org/facts/downloads/facts_figures_2015.pdf. Acessed June 2, 2015.
5. Rowe CC, Villemagne VL. "Brain amyloid imaging." Journal of Nuclear Medicine: official publication, Society of Nuclear Medicine. 2011;52(11):1733-40. Epub 2011/09/16. doi: 10.2967/jnumed.110.076315. PubMed PMID: 21917849.
6. Johnson KA, Minoshima S, Bohnen NI, Donohoe KJ, Foster NL, Herscovitch P, Karlawish JH, Rowe CC, Carrillo MC, Hartley DM, Hedrick S, Pappas V, Thies WH, "Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer's Association." Alzheimer's and Dementia: the journal of the Alzheimer's Association. 2013;9(1):e-1-16. doi: 10.1016/j.jalz.2013.01.002. PubMed PMID: 23360977; PMCID: 3733252.
7. Rice SL, Roney CA, Daumar P, Lewis JS. "The next generation of positron emission tomography radiopharmaceuticals in oncology." Seminars in nuclear medicine. 2011;41(4):265-82. Epub 2011/06/01. doi: 10.1053/j.semnuclmed.2011.02.002. PubMed PMID: 21624561; PMCID: 4406404.
8. Marquez BV, Ikotun OF, Zheleznyak A, Wright B, Hari-Raj A, Pierce RA, Lapi SE. "Evaluation of (89)Zr-pertuzumab in Breast cancer xenografts." Molecular Pharmaceutics. 2014;11(11):3988-95. Epub 2014/07/25. doi: 10.1021/mp500323d. PubMed PMID: 25058168; PMCID: 4224522.
9. Osborne JR, Green DA, Spratt DE, Lyashchenko S, Fareedy SB, Robinson BD, Beattie BJ, Jain M, Lewis JS, Christos P, Larson SM, Bander NH, Scherr DS. "A prospective pilot study of (89)Zr-J591/prostate specific membrane antigen positron emission tomography in men with localized prostate cancer undergoing radical prostatectomy." The Journal of Urology. 2014;191(5):1439-45. Epub 2013/10/19. doi: 10.1016/j.juro.2013.10.041. PubMed PMID: 24135437; PMCID: 4411555.
10. Gaykema SB, Schroder CP, Vitfell-Rasmussen J, Chua S, Oude Munnink TH, Brouwers AH, Bongaerts AH, Akimov M, Fernandez-Ibarra C, Lub-de Hooge MN, de Vries EG, Swanton C, Banerji U. "89Zr-trastuzumab and 89Zr-bevacizumab PET to evaluate the effect of the HSP90 inhibitor NVP-AUY922 in metastatic breast cancer patients." Clinical Cancer Research: an official journal of the American Association for Cancer Research. 2014;20(15):3945-54. Epub 2014/08/03. doi: 10.1158/1078-0432.CCR-14-0491. PubMed PMID: 25085789.
11. Dijkers EC, Oude Munnink TH, Kosterink JG, Brouwers AH, Jager PL, de Jong JR, van Dongen GA, Schroder CP, Lub-de Hooge MN, de Vries EG. "Biodistribution of 89Zr-trastuzumab and PET imaging of HER2-positive lesions in patients with metastatic breast cancer." Clin Pharmacol Ther. 2010;87(5):586-92. Epub 2010/04/02. doi: 10.1038/clpt.2010.12. PubMed PMID: 20357763.
12. Oosting SF, Brouwers AH, van Es SC, Nagengast WB, Oude Munnink TH, Lub-de Hooge MN, Hollema H, de Jong JR, de Jong IJ, de Haas S, Scherer SJ, Sluiter WJ, Dierckx RA, Bongaerts AH, Gietema JA, de Vries EG. "89Zr-bevacizumab PET visualizes heterogeneous tracer accumulation in tumor lesions of renal cell carcinoma patients and differential effects of antiangiogenic treatment." Journal of Nuclear Medicine: official publication, Society of Nuclear Medicine. 2015;56(1):63-9. Epub 2014/12/06. doi: 10.2967/jnumed.114.144840. PubMed PMID: 25476536.
13. van Dongen GA, Vosjan MJ. "Immuno-positron emission tomography: shedding light on clinical antibody therapy." Cancer Biotherapy and Radiopharmaceuticals. 2010;25(4):375-85. Epub 2010/08/17. doi: 10.1089/cbr.2010.0812. PubMed PMID: 20707716.


 April 22, 2024
April 22, 2024