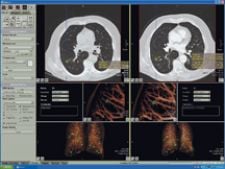
Vitrea solution integrates Vitrea workstation with R2's ImageChecker CT Lung CAD software for multislice CT.
(Updated content from 2015-2017 is at the bottom of this article)
The prevalence of lung cancer in the U.S., and the world for that matter, is a major public health and economic concern. Attributed primarily to cigarette smoking, lung cancer is usually diagnosed well into the latter stages of metastasis, meaning the deadly cancerous part of the tumor has already differentiated and separated from its origin and into the bloodstream. For decades, one of the primary diagnostic imaging tools to uncover lung tumors has been a chest X-ray.
Within the last decade, computed tomography (CT) has gained increasing recognition for its ability to form three-dimensional (3-D) images of the chest, resulting in greater resolution of nodules and tumor pathology. The disadvantage to CT-based screening is the high false-positive rate, which can be as high as 50 percent, depending on the study, and leads to unnecessary secondary invasive tests and greater patient anxiety.
Though early detection is certainly beneficial for patients, the relative advantages of X-ray over CT as the most appropriate standard of screening for lung cancer are still ambiguous. In fact, the National Cancer Institute (NCI) is sponsoring The National Lung Screening Trial (NLST), a lung cancer screening trial to detect a disease in asymptomatic patients using with X-ray or CT.
Lung Cancer X-ray
Due to the high prevalence of lung cancer among total cancer cases and the high mortality rate of the disease post-diagnosis, the prevailing thought is to identify visible nodules before they metastasize in order to dramatically reduce the death toll. According to the American Cancer Society (ACS), the predominant method of screening for lung cancer is to examine a patient’s chest X-ray along with a sputum analysis.
Although X-ray technology has advanced rapidly in recent years with the introduction of high-resolution digital X-rays, the smallest nodule size it can detect is limited to 1 to 2 cm. The false-positive rate ranges between 10 and 20 percent. Nearly every major comprehensive lung cancer screening study has failed to show that X-ray and sputum cytology reduce the mortality rate of lung cancer.
Two studies conducted in 1999 indicated that low-dose spiral computer tomography (LDCT) detected nearly six times as many nodules as traditional X-ray radiography. With resolution capabilities under less than 1 cm and the ability to generate 3-D views of the lungs, LDCT generated excitement as a high-quality substitute to X-rays. However, the LDCT’s high-sensitivity also generates a higher false-positive rate than traditional X-ray radiographs, with false-positive rates ranging between 20 and 50 percent. To date, there are still no authoritative studies that clearly identify LDCT as the best lung cancer-screening tool.
Identifying the most accurate tool for screening for lung cancer not only can save healthcare a tremendous amount of time and money, but more importantly, it can save more lives. With this endeavor in mind, the National Cancer Institute launched in 2002 an ongoing study to clearly define the correlation between screenings by X-rays or LDCT and mortality rates. The study includes 50,000 current or former smokers at 30 sites who are randomly assigned to either X-ray or LDCT examinations. The subjects obtain yearly screenings for three years, with secondary screenings such as needle biopsy and/or bronchoscopy performed on potential cancerous nodules. The study is geared toward including heavy smokers, defined by subjects who smoked three packs a day for 30 years, two packs a day for 20 years or one pack a day for 10 years, and subjects must be between the ages of 54 and 75, with no previous history of lung surgery and/or cancer. The trial follows patients for six to eight years and is anticipated to finish as early as 2009.
Researchers expect the screening will detect lung cancer in approximately five of every 100 patients enrolled, or a five percent incidence rate that could result in over 2,000 patients potentially being diagnosed with lung cancer. Radiologists will then assess the X-ray radiographs or CT scans and prescribe treatment options should cancer develop during the course of the study. The results of the NLST are much anticipated for both the patients and physicians since statistical data can corroborate the efficacy of using either X-ray and/or CT-based examinations for diagnoses and lung cancer mortality rates.
CAD-based Lung Cancer Examinations
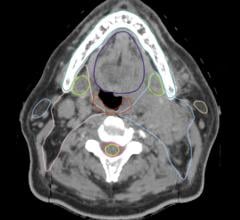
What may give CT a leg up on X-ray is Computer Aided Detection (CAD) for CT lung, software that highlights suspicious nodules in lung morphology and assesses nodule size changes over time to track progression of cancer therapy. CAD has also made its mark by demonstrating its capacity to provide radiologists with enhanced views of ultra-small pulmonary nodules from as little as 6 mm in size.
While promising, CAD is still a relatively new concept and some physicians and hospitals are skeptical of CAD’s benefits and its return on investment, especially if it is not reimbursed. However, as the number of images physicians are required to review has increased dramatically, and the number of radiologists remains relatively flat, there is a greater need for technology like CAD that can help increase the physician’s effectiveness and efficiency in identifying and managing potential abnormalities.
Solutions available on the market today include Siemens’ syngo LungCare and R2 Technology’s ImageChecker CT Lung Nodule application. As CAD’s performance in detecting lesions and nodules in the lung is not fully known, vendors are careful to point out that the intended use of their CAD solutions is as a second reader only – not a substitute. “CAD will increasingly become the standard of care with CT chest exams to detect and manage actionable lung nodules and pulmonary artery filling defects such as emboli to provide additional decision support,” indicated Terry Chang, director of CT CAD Marketing, R2 Technology Inc.
In recent studies involving a multireader receiver operating characteristic (ROC), potential nodules that were overlooked showed a 26 percent reduction with R2’s ImageChecker, as well as average reader improvement in radiologists to detect nodules between 4 and 30 mm in size. Another retrospective study showed that significant nodules were overlooked in 33 percent of cases, bolstering the need for technology that supports readers. Should CAD prove an effective diagnostic aid for CT lung exams, CT may likely outperform chest X-rays in screening for lung cancer.
How Well Does CAD Really Perform?
Investigators want to know if this is really true – could CAD become the gold standard for CT or X-ray exams? While lung CAD systems have proven promising as a second reader in detecting lung nodules, the critical question is how many of the detected nodules are really lung cancers?
Because the effectiveness of CAD in detecting lung cancer has not been fully investigated, the NCI has also put CAD under the microscope. In collaboration with the Foundation for the National Institutes of Health, the NCI is currently conducting the Imaging Database Resources Initiative (IDRI). By expanding the lung CT database of the Lung Image Database Consortium (LIDC) by 150 percent, and developing a new database for chest radiographs, the goal of IDRI, “is to rapidly create a public database of lung CT and X-Ray images that can be used by industry as a research resource to improve the optimization and evaluation of computer aided diagnosis (CAD) products to improve the clinical management of lung cancer.” The databases will allow for meaningful comparisons between CAD methods, identify promising CAD techniques, and may prompt innovation and the development of new chest CAD software at a lower cost.
“The sheer number of images being generated in a thin-slice spiral CT study is making it extremely difficult for radiologists to look for small nodules in every image,” he said. “CAD is needed as a practical necessity. One hindrance to CAD development has been the lack of a high-quality, ground-truth, standardized database. Our second motivator is to provide that database,” said Laurence Clarke, Ph.D., chief of the imaging technology development branch of NCI’s Cancer Imaging Program.
The database is designed to aid in managing the enormous volume of data produced by CT lung imaging in hopes that CAD algorithms will aid in the task of early detection and treatment of lung cancer. With the database nearing 400 cases, the LIDC project should be completed soon and the information available for public research use in the third quarter of 2006. At that point, doctors may have a clearer picture on what imaging method – X-ray or CT – is the most effective for screening for lung cancer.
Related Lung Cancer Imaging Content:
The American Lung Association creates LUNG FORCE
Mesothelioma Imaging and Diagnostics, What to Look For
Medicare CT Lung Cancer Screening Coverage a Victory for Patients





 April 23, 2024
April 23, 2024