GE Healthcare offers the Discovery PET/CT 600, which is suitable for oncology, including radiation treatment planning and monitoring.
Multimodality imaging in medicine can provide a physician with tools for making an accurate diagnosis prior to making treatment recommendations and helps the physician to lessen the potential for restaging, simplifying the image evaluation process and improving patient care in the future. The benefits also can be applied to the improvement of imaging in clinical trials, where precision and standardization is a necessity.
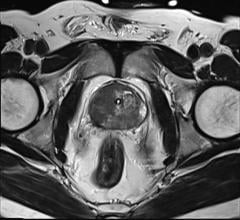
For many diseases, including cancer, heart disease and certain brain disorders, the current and typical imaging process requires the acquisition of both positron emission tomography (PET) and computed tomography (CT) scans. PET scanners typically measure metabolic activity, while CT scanners highlight anatomical features. As these modalities are acquired independently, there frequently is an added burden on the patient to have to travel to separate imaging facilities, and it requires more time for the physician to evaluate the scans.
Often a complete evaluation requires the physician to view co-registered PET and CT fused images. The challenge in this approach lies in accurately superimposing a patient’s anatomy across different modalities when images have been acquired in separate sittings, with unstandardized parameters, and by different technologists.
Recently, this issue has been shown to be alleviated by the increased availability of multimodality scanners capable of acquiring complementary imaging sets in one sitting. Clinically, the best example of multimodality imaging thus far is in the use of PET/CT scanner hybrids, which combine the strengths of the two well-established imaging modalities to more accurately diagnose, localize and monitor disease. The risk to poor superimposition of separate imaging is mitigated and, importantly, the hybrid PET/CT process lessens encumbrance on the patient by simplifying the scanning scheduling process.
One main advantage of a PET/CT scanner is that it uses the CT images (as transmission images) for attenuation correction of the PET data, rather than relying on a rotating transmission rod source. PET/CT scanners are able to perform the registration of the transmission images in extremely short times (less than a minute), with the PET study acquisitions performed immediately after. Upon reconstruction, both the PET images and the CT images are displayed side by side and overlaid.
Use of the CT scan reduces the total PET acquisition time, which translates into increased patient comfort and cooperation. The availability of high-quality transmission images also leads to a more precise localization and interpretation of the hypermetabolic disease areas. While other indications benefit from PET/CT scans, today’s oncology procedures far outnumber all other clinical indications.
Current Scanners and Recent Advances
The first hybrid anatomical-functional imaging system was a dual-head scintillation camera combined with a low-power X-ray tube and detectors. In the beginning, hybrid scanners had minimal integration of any hardware, and the vendors mainly combined an existing high-end PET scanner with a two- or four-slice CT scanner. These essentially separate components were housed inside a single gantry or, in some cases, in two separate gantries.
In the past eight years, however, PET/CT designs from all vendors have evolved, mainly because of improvements in the performance of the individual CT and PET components and enhanced software integration. The need for high-speed CT, driven mainly by the cardiology market, has seen the original two- or four-slice scanners replaced with eight-, 16-, 40- and 64-slice models, and developments in PET hardware have resulted in improved detection speed and efficiency.
PET/CT design is continually being innovated. The newer technology enables more precise measurements of metabolic processes and data quantification, including assessment of neurologic disease, cancerous tissue and cardiac blood flow (perfusion).
Certain scanners have platforms designed to configure scanner performance and financial costs. Several of the scanners include accommodations for radiotherapy positioning devices, offering larger (70 cm) field-of-view for both PET and CT to help facilitate accurate radiation treatment — especially important for obese patients and patients where skin surface/lesions are being evaluated.
Similarly, the newer scanners are able to be used on more patients, as they feature a wider imaging bed that can accommodate patients who weigh up to 500 pounds. They also feature a larger scan range to fit taller patients comfortably on the table for a complete head-to-toe study, without interruption or repositioning.
Other newer scanners use special protocols to help reduce CT radiation exposure in fludeoxyglucose (FDG) oncology pediatric exams to meet ALARA (as low as reasonably achievable) guidelines. A 3-D modulation algorithm maintains CT image quality and is beam optimized for dose efficiency, reducing it by 40 percent. Many scanners are designed to bring the benefits of PET/CT to more oncology patients.
Unique imaging technologies include 20-slice adaptive CT, standard PET time-of-flight (TOF), HD.PET for uniform resolution across the entire field-of-view and HD.chest to reduce blur created by respiration during PET/CT studies. These systems are ideal for smaller markets, such as community hospitals, small imaging centers and emerging markets exploring hybrid imaging for the first time.
However, these scanners also offer scalable upgradability. The number of CT slices can be increased to 40, 64 or 128 to improve performance, while the standard PET field-of-view (FOV) of 16.2 cm can be upgraded to 21.6 to improve imaging capabilities. Dose-reduction technologies, specialty clinical engines, workstations and/or thin-client solutions are also upgradable options.
Other newer scanners facilitate the use of PET in radiotherapy planning by streamlining tumor detection, staging and simulation. They also monitor therapy response, featuring a consistent wide bore opening for both PET and CT, which allows patients to be positioned in the same manner for both simulation and therapy. This type of setup allows for greater patient comfort and increased flexibility in positioning.
TOF technology for PET is designed to enhance image quality by reducing image artifacts and providing higher sensitivity. Most recently, a new generation of scanners has been designed based on time-of-flight, utilizing avalanche photodiode detectors that will further improve technical performance. The resulting images help clinicians better detect and locate lesions to increase diagnostic confidence and preserve healthy tissue during treatment.
Rapid Evolution of PET/CT Technology
The value of PET/CT using FDG for diagnosis and staging is well established for a wide range of clinical sites. The hybrid technology itself has had an impressive evolution since its inception more than 10 years ago.
While the spiral CT scanners have evolved from two- to 64-slice devices, the PET scanners have also seen an improved spatial and temporal resolution, sensitivity and contrast. The impact of 2-D versus 3-D whole body imaging has decreased the scanning time without sacrificing image quality. Additional advantages include faster patient throughput; CT and PET scans can be completed in 30 to 45 minutes, whereas a PET scan alone can take up to 60 minutes. Another advantage is higher patient and technologist compliance due to shorter scanning times, and routine and near-instantaneous image fusion made possible by simultaneous imaging, with constant geometry and patient positioning at a single examination performed on the same scanning bed.
The significantly improved precision of co-registration of anatomy and function has resulted in improved reader confidence in lesion detection and localization, as well as characterization, leading to a marked reduction in equivocal findings. The most extensive use of FDG PET/CT to date has been for diagnosing and staging in oncology, and the published data suggest a rapid introduction of PET/CT diagnostic systems into routine oncological practice.
The hybrid technology has widely been accepted by oncologists all over the world, thereby validating its excellent technical performance, clinical utility and scientific potential. So much so, in fact, that the main imaging vendors in the market are no longer producing standalone PET scanners and, consequently, only PET/CT machines are now sold new into the market. As a consequence of the great improvements in technology and growing evidence that a PET/CT examination demonstrates superior diagnostic performance over separate PET and CT exams that are interpreted side by side, there has been significant growth in the usage of PET/CT in clinical practice.
Even though more data is needed, clinical experience thus far has demonstrated that PET/CT has a substantial impact on patient management and the identification of appropriate surgery, radiotherapy or alternate treatment. In therapy planning, PET/CT can better define the target and the strategy of the treatment and can help reliably identify appropriate subsets of patients who will likely not respond to therapy. This approach can prevent unnecessary rejection of various treatment options through the observation of only targeted patients, rather than looking at the overall results of a large study population. Thus it is possible for patients to avoid ineffective and toxic treatments and instead get the benefits of an optimized therapy plan.
The costs associated with PET/CT are relatively high compared to other imaging procedures. But since PET/CT has been found to better assist physicians in identifying appropriate treatment, the extra cost translates into improved quality of care. Also, the cost of other therapeutic interventions, which may not be needed with the use of PET/CT, is much greater than those associated with diagnostic imaging procedures.
PET/CT in Clinical Trials
As PET/CT scanners are becoming more common in clinics, the technology is also being implemented into early phase clinical trials. In a recent Perceptive Informatics-managed early phase study with four sites, each had access to PET/CT scanners, which were used to acquire images for independent image review.
Key criteria, such as RECIST 1.1 (Eisenhauer EA, et al) and IWG-NHL 2007 (Cheson BD, et al), allow for a limited integration of FDG-PET with the anatomical CT (or magnetic resonance [MR]) imaging. While fused PET/CT images are not required in this setting, high-quality co-registered images are helpful in scan interpretation and often expected by reviewers and sponsors.
It is the (non-validated) assessments in early phase settings, however, that appear to benefit the most — definitions of regions and volumes of interest, especially for mean standardized uptake value determination, can benefit greatly from a more reproducible approach. Standardization and precision are essential pieces of a successful clinical trial and the chief goal of a central imaging vendor.
Thus, since the data show that PET/CT scanners are being used more frequently in clinical care, it is essential that this innovation be applied regularly in clinical trials as well. Hybrid PET/CT is the logical and appropriate replacement for standalone PET and CT imaging in future clinical trials.
Neru Munshi, Ph.D., medical research associate, medical imaging, Perceptive Informatics, provides medical expertise in study design, protocol standardization and customization of analysis software tools for oncology clinical trials. Munshi completed post-doctoral training at Harvard Medical School, where she conducted preclinical studies on understanding the molecular pathways involved in cancer cell growth and proliferation. She has published in the field of signal transduction and cancer biology. Perceptive Informatics, a subsidiary of Parexel, provides advanced technology solutions, including medical imaging, to facilitate clinical development.
References:
1. “A Guide to Clinical PET in Oncology: Improving Clinical Management of Cancer Patients.” International Atomic Energy Agency 2008.
2. Townsend, DW. “Positron Emission Tomography/Computed Tomography.” Semin Nucl Med 38:152-166; 2008.
3. Eisenhauer EA et al. “New response evaluation criteria in solid Tumours: Revised RECIST guideline.” European Journal of Cancer, 45 (2009) 228-247.
4. Cheson BD et al. “Revised response criteria for malignant lymphoma.” J Clin Oncol 2007 Feb. 10;25(5):579-86.




 April 17, 2024
April 17, 2024