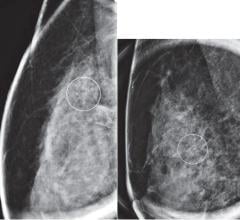
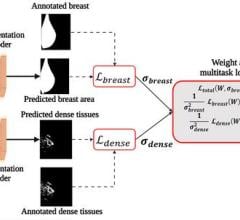
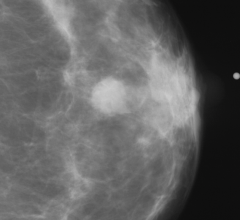
Since the release of the Digital Mammographic Imaging Screening Trial (DMIST) results in September 2005, there is little controversy over the benefits of digital imaging in detecting breast cancer. The study found that digital imaging was as accurate as film in detecting breast cancer and 28 percent more accurate in women under 50 and in women with denser breast tissue. Also, full field digital mammography (FFDM) was more likely than screen-film mammography (SFM) to detect invasive carcinomas and medium- to high-grade ductal carcinoma in situ, tumors that when detected and treated early are essential to saving lives.
Despite the obvious benefits, almost a year and a half later only 12 percent of breast imaging facilities across the nation have acquired digital imaging screening devices. The reason for the lag in acquisition is in part due to the high cost of purchasing, operating and maintaining digital imaging equipment. Purchasing a digital mammography unit costs about $400,000 and requires replacing conventional X-ray machines used for standard SFM. Add to that the operating costs, which run approximately $135,000 a year in comparison to $24,000 for a standard X-ray mammography system. In addition, users of digital radiography have reported that interpreting the digital images takes significantly longer than interpreting film, suggesting that slower productivity could mean lower profit margins.
In the endeavor to provide a more cost-effective way for facilities to acquire digital imaging, both Eastman Kodak and FUJIFILM have introduced economical solutions with Computed Radiography (CR) systems for mammography. Fuji is the first vendor to offer a FFDM system based on computed radiography with its Fuji Computed Radiography for Mammography (FCRm). FCRm does not require replacing the existing mammography unit, which simplifies the conversion to digital for facilities. Film cassettes are replaced with FCR cassettes, and after the exam, the cassettes are digitally processed and the resulting images sent to a computer workstation configured with high-resolution monitors. Up to three exam rooms can be converted to digital per system, and at about half the cost per room as existing FFDM systems.
Kodak also boasts its Kodak DirectView CR, which is currently undergoing the final phases of regulatory review within the U.S. DirectView is similar to Fuji’s FCRm in terms of lower costs, said Stephen Archer, worldwide marketing director for Kodak’s mammography solutions business.
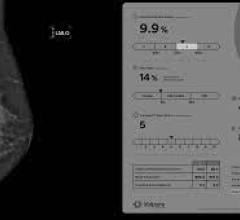
IT solutions for managing growing image data sets are critical as mammography converts to a digital format. Recently, Merge eMed rolled out MergeMammo, a vendor-neutral workstation software application for digital reading and review of mammography images that displays images from mammography, MRI, ultrasound and other modalities on one workstation. Reportedly compatible with any computer-aided detection system, the application strives for seamless integration.
The results from the DMIST trials showed that digital imaging holds much promise for the future health of women. The question is no longer whether digital is better, but instead how to make the technology accessible and utilitarian. Since the DMIST news went public just a year and a half ago, technology has come a long way in helping the medical community transition to digital.
Feature | January 22, 2007 | Amy Ballard, MEd
The question is not whether digital is better, but how to make digital cost effective and accessible.
© Copyright Wainscot Media. All Rights Reserved.
Subscribe Now


 April 02, 2024
April 02, 2024