April 30, 2015 — Two new studies show that increasing the dose of radiotherapy given to children with an intracranial ependymoma, a form of cancer of the central nervous system, can significantly improve their survival. Results of both studies were presented at the third European Society for Radiotherapy and Oncology (ESTRO) Forum in Barcelona, Spain.
Malignant ependymoma, which develops in the cells that line the hollow cavities of the brain, is normally treated with a combination of surgery and radiotherapy, sometimes with the addition of chemotherapy. Since 2004 a dose of 59.4 Gy has been recommended for pediatric cases worldwide, as opposed to the lower (54 Gy) dose that was in use previously; the studies say adding a radiotherapy boost to this can improve outcome yet further in selected cases.
Ependymoma is the third most common brain tumor in children. With surgery and radiation therapy, the overall five-year survival rate is approximately 70 percent, but individual prognoses differ considerably according to a number of factors — age, extent of surgery, and radiotherapy technique and dose.
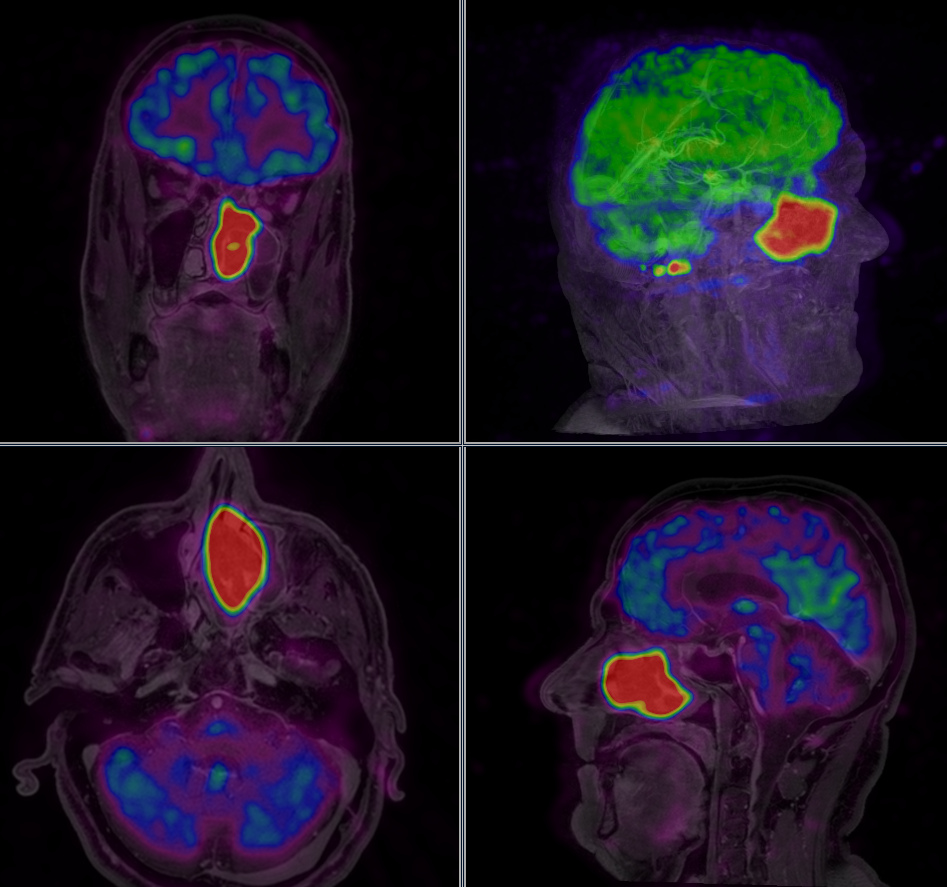
Lorenza Gandola, M.D., head of the Pediatric Radiotherapy Unit at the Fondazione IRCCS, Istituto Nazionale dei Tumori, Milan, Italy, described how her team developed an innovative strategy for children who still had measurable intracranial ependymoma after surgery. In addition to the 59.4 Gy radiotherapy dose to the tumor bed, they added a boost of 8 Gy, divided into two fractions, to the tumor residue. The researchers used a combination of highly sophisticated radiotherapy techniques in order to deliver the radiation dose directly to the remaining malignant tissue while sparing normal brain tissue as much as possible. Twenty-four eligible children (median age 4.5 years) out of the 143 in the Italian project received the radiotherapy boost and 15 of them are still alive without disease progression at a median of 51 months after diagnosis.
"Our strategy contributed significantly to obtaining durable local control of disease in these children, and this is more striking because they already had a poorer prognosis after surgery," Gandola said. "The hypofractionated radiotherapy boost approach represents an effective alternative to surgery in cases where further surgery cannot be performed without the possibility of causing severe and perhaps life-long damage to the child."
No deaths related to the treatment or major toxicity have been reported in the boost group, the researchers said. The technique will now be the subject of an international clinical trial, to be carried out under the auspices of the European Pediatric Oncology Society (SIOP) and planned to start later this year.
"We believe that our research has the potential to improve outcomes in children with poor prognosis ependymoma, and we hope that the SIOP trial will confirm them further to the benefit of such patients," Gandola concluded.
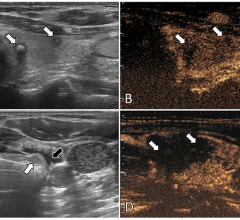
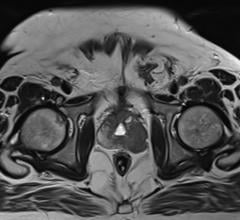
In another presentation, Anne Ducassou, M.D., from the Institut Claudius Regaud, IUCT-Oncopole, Toulouse, France, discussed findings from a study of all 177 children treated for ependymoma in France between 2000 and 2013. The children ranged in age from 1-23, with a median age of five. The researchers studied the characteristic of their disease as revealed by magnetic resonance imaging (MRI) scans, and specifically in those related to metabolism — for example perfusion (the blood flow created in the tumor), and the diffusion of intercellular water molecules, which also reflects the number of cells in the tumor. "We wanted to know whether these metabolic characteristics might have a role in the prognosis of local control of disease and in survival, and whether they might also be able to help us predict relapse, where the disease returns or reoccurs after a period of improvement," Ducassou said.
All radiation oncologists in France who had treated pediatric patients with ependymoma provided information to Ducassou's team. The researchers found that children with localized disease who had been treated with the high radiation dose of 59.4 Gy, in use since 2004, did better than those who had received the lower dose in use until that date. Of the 177 patients included in the study, the estimated overall survival and progression-free survival (where the disease remains but does not get worse) were 90 percent and 67 percent for patients who received a dose above 54 Gy, compared with 79 percent and 52 percent who received a lower dose.
"Our work, which involved a large number of children with ependymoma, has confirmed that the treatment we carry out today is better than it was a few years ago, but there is still much work to be done. For example, we found that children younger than three, and those with more aggressive disease had a poorer outcome, and we need to look further at how we can improve their treatment, as well as identifying other children at high risk of relapse," Ducassou said.
Prof. Philip Poortmans, president of ESTRO, commented: "Cancer in children is luckily rare but, when diagnosed, has a major effect of the lives of not only the patient but also the parents and other people close to the child. Recently, research in childhood cancer has focused mainly on the avoidance of late side effects. However, in cases like that of ependymoma, many patients are still not cured and subsequently die from their disease. Therefore it is important to be able to be able recognize accurately those children who are at high-risk for recurrence, and to intensify their treatment.
"Both studies presented here demonstrate that a clear dose-effect relationship exists for tumor control and survival. While the increase from 54 to 59.4 Gy that was adopted first improves disease control and survival in a population-based study, a new study is planned to confirm the results of increasing the dose by a further 8 Gy, delivered with highly directed radiation therapy techniques that give a very localized dose to the target volume with a low dose to the surrounding normal tissues. We hope that this will bring about even better outcomes for these children."
For more information: www.estro.org


 April 17, 2024
April 17, 2024