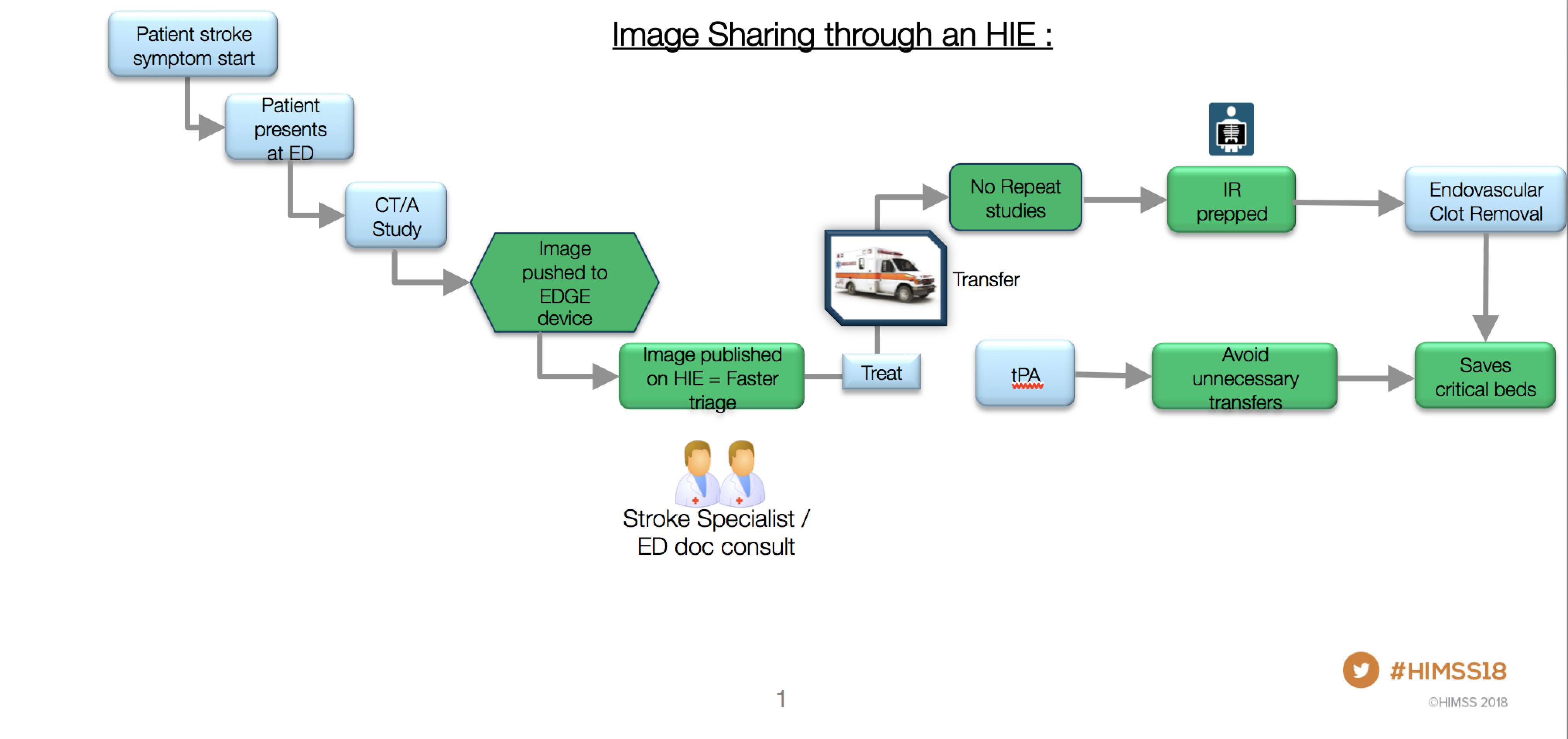
How image sharing through a health information exchange benefits patients while saving time and money is depicted in this slide shown at HIMSS 2018. Graphic courtesy of Karan Mansukhani.
A regional image exchange system is saving lives and reducing radiology costs in Maryland by improving the efficiency and effectiveness of diagnosing and treating stroke patients.
The image exchange, part of a statewide health information exchange (HIE) called CRISP (Chesapeake Regional Information System for our Patients), not only accelerates the diagnosis of stroke patients, but also allows their treatment to be individualized. Further, it affords the option for transfer to a comprehensive stroke center where patients can receive advanced therapy.
This one-two punch of diagnosis and treatment is particularly important for rural hospitals in Maryland that do not have experts to interpret computed tomography (CT) images or the resources to execute advanced therapies. “We have learned that we can really improve lives,” said Michael S. Phipps, M.D., MHS, director of the University of Maryland’s Brain Attack Center, which serves as one of the Maryland Comprehensive Stroke Centers. “When we are able to view images quickly, we can make better decisions faster. That changes outcomes.”
Improving Care
In a presentation at 2018 Healthcare Information and Management Systems Society (HIMSS) conference, Phipps and CRISP program manager Karan Mansukhani presented preliminary data about the operation of the CRISP-based image exchange. Over the last three years, patient transfers to the comprehensive care centers have risen from 43 in 2015, to 66 in 2016, to 91 last year. Repeat imaging studies were zero in 2015, eight in 2016 and five last year.
CRISP allows the display of current images in the context of priors and other clinical data, including laboratory values. This accelerates the diagnostic process and dramatically reduces the time to treatment, Mansukhani said.
“The data that we have collected so far shows that we are able to save 56 minutes on average in time to decision,” he said. “Because stroke treatment is time sensitive, getting images (and data) in front of a specialist is critical.”
This point is underscored by the higher percentage of patients who score better on the “modified Rankin” score, which indicates disability due to stroke. Ninety days after the stroke, according to Mansukhani, 28 percent of patients showed a good outcome after the image exchange technology became operational. This contrasts with 20 percent of patients who showed a good outcome before the technology, he said.
How It Works
Stroke images from participating acute care hospitals in Maryland and Washington, D.C., are transmitted for interpretation by a CRISP-based team comprised of a stroke specialist, neuroradiologist and stroke resident. Following diagnosis, the stroke specialist collaborates with emergency physicians to triage patients and plan treatment.
The images are taken using CTs installed at the regional hospitals. A DICOM-enabled edge device, integrated with a hospital server, queries the on-site picture archiving and communication system (PACS) for the CT images, caches and then transmits them through the HIE for interpretation.
Why Stroke
Stroke is the fifth leading cause of death in the U.S.; the third leading one in Maryland; and the chief cause of serious, long-term disability in the U.S. Ischemia caused by clots accounts for 87 percent of all strokes. Advanced methods for clot removal, notably the 2013 development of advanced suction catheters, have substantially improved patient outcomes, according to Phipps.
Conversely, hemorrhagic stroke comes from the rupture of a blood vessel in the brain. Blood accumulation increases pressure, which causes blood loss to nearby tissues. Patients are treated by controlling the bleed and relieving the pressure.
Symptoms alone do not define the type of stroke. The only way to determine the type — and the most effective treatment — is the accurate interpretation of brain scans, Phipps said. Many community hospitals lack the necessary diagnostic and therapeutic resources, much to the disadvantage of the stroke patient. Effective treatment must begin within six hours of symptoms, he said. “Ischemic strokes may only allow treatment for a short time. Time is brain.” The sooner the reperfusion, according to Phipps, the better the outcome.
In 2015, research published in the Journal of the American Medical Association (JAMA) showed that more than half — and up to more than 70 percent — of patients reperfused between 4 and 4.5 hours since the onset of stroke symptoms showed good clinical outcomes after 90 days. This compared to between 20 percent and slightly more than 40 percent of patients who showed similar outcomes when reperfused between 5.5 and 6.5 hours.
HIE Imaging Sharing
Data gathered by Mansukhani and Phipps show that the HIE-enabled electronic image exchange is substantially better than image sharing that relies on physical media. Inefficiencies associated with these media, such as CDs, may lead to repeat CT studies, Mansukhani said.
When establishing electronic image sharing within an HIE, they recommend leveraging “champions” within these exchanges who can ensure that the exchanges are set up and operate efficiently and effectively. To be effective, these exchanges need to work with PACS administrators and radiology technologists, said Mansukhani. “Without their hard work, our lofty goals would be beyond us.”
Greg Freiherr has reported on developments in radiology since 1983. He runs the consulting service, The Freiherr Group.



 April 22, 2024
April 22, 2024