Two-dimensional (2-D) digital mammography has been the gold standard for the first line of defense in breast cancer. Yearly mammograms are suggested for women beginning at age 40 and continuing as long as women are in good health. And while 2-D mammograms appear to be sufficient for many women who report no findings on their mammograms, there is much controversy surrounding what the second line of defense should be for those women who require a second look.
Second looks are not specific to mammography, and occur in all aspects of imaging. If physicians spot abnormalities, they will order a second test, oftentimes using a different imaging modality, to confirm or negate prior results. The complication with women’s imaging arises because there is no best standard for second looks. According to Monique Rasband, author of the KLAS report, “Women’s Imaging 2013: Measuring the Options,” there is not a perfect solution that is going to find cancer 100 percent of the time. “It just simply does not exist, and the breast is very complicated,” she stated. Due to complicated breast tissue, the imaging modality of choice for second looks largely depends on provider opinion, the case-by-case situation and what is seen in the first mammogram.
Tomosynthesis as an Option
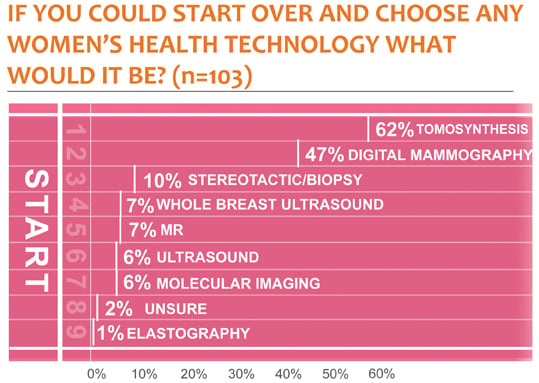
One way that physicians are addressing the issue of second looks is by providing what many consider a better first look. According to the KLAS report, 62 percent of physicians, directors, nurses and managers stated that if they could start over with the purchasing for their department, they would choose tomosynthesis — a 3-D mammogram.[1] (See If You Could Start Over figure.) Rasband said the popularity of tomosynthesis is due to its ability to reduce the number of false positive callbacks when compared to standard 2-D mammography alone. She said that according to the people interviewed for the KLAS report, tomosynthesis roughly reduced false positive callbacks by about 30 percent on average.
This presents a great benefit for those women who have had an abnormality spotted on their standard mammogram, because getting back in to see a physician for a second look can be challenging. With long waiting lists and conflicting schedules, it is possible for women to go weeks before getting an appointment. This leads to days and weeks of anxiety for some women as they wait without knowing their status. Many of these women suffer from this anxiety only to find out that after a second look, the initial reading was a false positive. For this reason, false positives are a big issue, and for many providers tomosynthesis poses an effective solution.
The Flip Side of Tomosynthesis
However, like most aspects of women’s imaging, tomosynthesis does not come without its fair share of critics. One note of criticism is that the benefits of tomosynthesis have not been fully substantiated by clinical trials. There are still many clinical trials being performed to provide further clinical evidence to the test’s true benefits. This, coupled with the fact that tomosynthesis exposes patients to additional radiation dose and that the exam is not covered by insurance, has lead many providers to decide that at the moment, it is not worth it. “There are those who don’t use tomosynthesis because they say it’s not really proven and they don’t want to expose the patient to more radiation dose,” said Rasband.
Ultrasound for Women’s Imaging
Another popular option among physicians and patients is ultrasound. Ultrasound is popular because it is a more cost-effective solution for providers and a no-dose option for patients. “A lot of people like ultrasound because it is no-dose and it will be very safe for the patient, plus the technician can really zero in,” said Rasband. Unlike standard mammography, which just gets a picture, ultrasound allows providers to go in and maneuver the image.
Whole breast ultrasound is also beginning to compete with general ultrasound because it is dedicated to breasts. “We have seen a lot of uptake in the adoption of whole breast ultrasound,” said Rasband. “There’s not nearly as many units out there, but it will be interesting to see in the future if that is something that we will see go up over time.” To date, both Siemens and GE have developed whole breast ultrasound systems.
While whole breast ultrasound is a promising technology, it has not taken off quite yet. “Even GE, with the largest number of installs, only has about 20 or 25 in the U.S.,” Rasband said. It is also important to note that ultrasound in general can miss cancer and is generally not used alone, but rather as a complement to a standard mammogram.
Factoring in Healthcare Costs
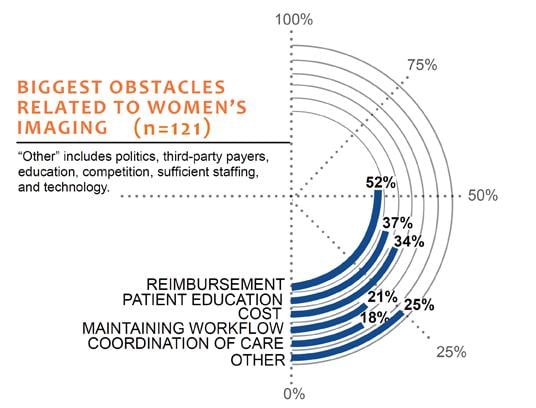
One major factor that goes into deciding what imaging modality a provider chooses to use is the cost. According to Rasband, money is tight for many providers. And because healthcare is not in the best condition right now in terms of reimbursements, going out and investing major dollars in technology or software upgrades for which providers are not going to get reimbursed may not be a priority. “You have providers who say we have an ultrasound that’s broken down, our CT is old and all these other issues. So, how do you choose to do a tomosynthesis upgrade when you have other needs and tomosynthesis is something that is still not reimbursed?” she said. “It definitely becomes political and sort of a pecking order so to speak.”
However, there are providers who have said that investing in these technologies and software upgrades is worth it because they get many more referrals in other areas and a lot more mammograms. For some providers who choose to spend money on additional imaging modalities, it is paying for itself and bringing more business because patients prefer to go to a facility that may have a 30 percent higher chance of finding something or identifying false positives.
Dense Breast Discussion
Another issue that is playing a big role in second looks in women’s imaging is the discussion of dense breasts, which has recently been brought into the national spotlight. It is estimated that between 30 and 40 percent of women in the United States have dense breasts.[2] Dense breast tissue makes it difficult to identify breast tumors on standard mammography exams until very advanced stages, and because of this dense breasts are a strong independent factor for breast cancer. Many states have begun passing legislation requiring radiologists to tell women if they have dense breasts, and to inform them of the benefits additional screening may offer them.
While the education that patients are beginning to receive will have positive effect on patients, dense breast legislation has also become a controversial topic within women’s imaging. One area of controversy is the lack of standardization in the education and care of women with dense breasts across the nation. Rasband said that among states that are letting their patients know their density status, some are only requiring that providers tell patients if they have dense breasts. Other states are requiring insurance to pick up the cost of supplemental screening if a patient has them. And still other states are saying that even if a patient has dense breasts, if additional screening is desired, the patient has to pay out-of-pocket because insurance will not cover it.
“The entire country is very divided,” said Rasband. According to the KLAS report, however, “there is some momentum toward a standard reimbursement for ultrasound.”
Because the dense breasts discussion and the state-by-state legislation are relatively new, there have also been workflow issues in implementation. In the KLAS report, one director stated, “We aren’t sure what processes to put in place to get this important information to our patients without bogging down what we already have to do.”[1]
One of those processes includes who should actually be responsible for disseminating such vital information. Rasband said that patients do not usually talk to radiologists even though the radiologist is the expert in reading breast exams.
“Your OB or primary physician is the one who is telling you that you have dense breasts, but the radiologist is really the one who knows yea or nay,” she said. “At this point in some cases it’s a positive effect to the patient, but in terms of workflow and processes, because it’s new, the education around it and the resources in some cases is also a negative because it’s a piece that’s adding into the workflow.”
References:
1. M. Rasband, “Women’s Imaging 2013: Measuring the Options,” KLAS Research
2. W. Nyanue, “Breast MRI Benefits from Research,” Imaging Technology News 2013: 53:11


 April 16, 2024
April 16, 2024 








